'System logic'
'System logic'
This chapter closes the loop of the 'Logic of medical language' to introduce a diagnostic model in the field of masticatory functions that combines the conceptuality of system logic with quantum mechanics. The statistical mathematical models of a system logic, therefore, cannot be subjective, nor approximate, much less vague and non-formal in the context of the clinical model. To obtain these characteristics it is necessary to consider the basic concepts of 'Systems Theory'.
The irrefutable diagnostic breakthrough in most medical disciplines lies in bioengineering, technological advances and specifically systems theory. It allows to verify the state of a system by comparing output variables generated by input variables. This huge step forward lies in the introduction of the trigger concept. Bioengineering in the trigeminal electrophysiological context has allowed the use of a series of triggers (transcranial electrical stimulation, transcranial magnetic stimulation, mechanical stimulation of the trigeminal district) that let us test the system with a much higher resolution than that in which the system is tested without responding to an external trigger. Another key element is that the trigger model is able to provide a snapshot of the system state many years before an obvious pathological clinical sign occurs.
In this chapter we will explain some basic steps to take in modeling diagnostic methods following systems theory.
Article by Gianni Frisardi · Giorgio Cruccu · Alice Bisirri · Pier Paolo Valentini · Flavio Frisardi · Irene Minciacchi
|
Foreword
Why did we come to the 'System Logic'? The steps are neither trivial, nor personal, and in order to perceive the added value of the 'System Logic' we cannot help but mention two essential reasons that have marked this path: that of dental clinical indices and of logic of medical language.
Dental clinical indices
There are 'Indices' that can be considered elements of System Logic as objective data, such as the 'Henderson-Hasselbalch equation' (for blood pH analysis) and other 'Indices' developed in the medical field in disparate disciplines.[1][2][3]
A test, a normative reference datum or an 'Index' (as well as a 'Constant') are strategies related to mathematical-statistical models that generate data. These data are mandatory for the accuracy of the diagnosis, for the differential diagnosis as well as for the therapeutic guidelines. On these reference data, in the times of scientific dental history, implementations and modifications have been generated but also uncertainties and beliefs that in the form of axioms or schools of thought have set guidelines that are not always scientifically justifiable, and sometimes untrue.
In literature
We can take into consideration the data reported in the literature regarding the 'Indices' studied on patients suffering from 'Temporomandibular Disorders'[4] or enter more specifically about masticatory rehabilitations and verify the 'Clinical Indices' topic in orthodontic disciplines.[5]
In a recent article by Andrea Scribante and collaborators,[6] for example, the following paragraphs are deduced:
- The introduction states that the evaluation of the outcomes of orthodontic treatment has traditionally been carried out using the experience and subjective opinions of clinicians.[7] In this first paragraph the limit of the concept expressed is understood and that is a diagnostic test and / or therapeutic guideline should never be scientifically weighed using subjective parameters.
- However, since the 1990s, specific indices have been developed to objectively evaluate health outcomes by analyzing the quality of treatment.[8] These indices compare pre- and post-treatment data to determine the outcome of orthodontic therapy[9] and to improve the quality of future treatments.[10] This second scientifically acceptable paragraph highlights the purpose of the 'Indices' and that is the pre- and post-comparison - but who says that the post is in a state of 'normocclusion' and the pre in 'malocclusion', the dental alignment?
- The most commonly used index for evaluating orthodontic success is the Peer Assessment Rating Index (PAR), which was developed to measure how far a patient deviates from normal occlusion and alignment.[8] This index was used to evaluate the effects of therapy in different circumstances: the use of fixed and mobile devices,[11] the comparison of orthodontic treatment between private practices and orthodontic schools,[12] the evaluation of occlusal stability after orthodontic treatment,[13] early treatments[14] and results of orthognathic surgery.[15] We have to consider that PAR would not indicate the healthy or the sick, normocclusion or malocclusion depending on whether it moves away from the cutoff but in the face of a series of incoming characteristics it would return a broad spectrum response (Index), valid for orthodontic treatments and orthognathic. This state of mind is legitimate but the clinicians have to be careful because the input variables (the 'Constructors') of the model or input, may not be related to the reference context or there may be other hidden variables that would invalidate the result itself. We will appreciate these assertions more strongly in the exposition of the chapters of Masticationpedia.
The fact is that the primum movens of the studio of Andrea Scribante and collaborators is concentrated in the following point:
(Limitative .... the index can have an accuracy and truthfulness in dental alignment but not to validate a normocclusion, this latter assertion is much more complex to formulate and certainly cannot be reduced exclusively to an 'Occlusal observable'.)
Spyridon N. Papageorgiou[16] in a very interesting study exposes a corageous statement that confirms what has just been exposed:
- Noticeable long-term occlusal changes are observed in the post-debond, which mostly favor better settlement. The higher quality finish at the debond significantly influenced the possibilities for improvement. However, setting a cutoff score to denote treatment excellence has shown considerable instability over time.
Other authors state that relapse after orthodontic treatment can also occur in cases with good functional occlusion.[17]
Further considerations
The etiology of recurrence is neither fully understood nor can it be fully predicted from a single factor,[18] but includes factors such as the response of the traction and deconstructed periodontal fibers,[19] physiological maturation of the human dentition which affects its width, length or perimeter[20], alterations of the craniofacial complex[21] and parafunctions.[22]
Retention of treatment results is therefore considered to be one of the most difficult problems in orthodontics, and relapses, especially of the mandibular incisors, could also be observed with the use of retention devices after debonding.[23] Most of the existing post-treatment stability studies evaluate short-term relapses of the anterior region by primarily measuring the irregularity of the incisors after extractive or non-extractive treatment and compare different retention patterns. These studies largely use the Peer Assessment Rating (PAR) index[24] which is not a trigeminal electrophysiological analysis approach in considering 'Normocclusion' much less the details of a well balanced occlusion (such as contacts, inclinations and alignment of each tooth) or changes in retention only in the short term.[25]
To the authors' knowledge at the time of publication of their study, only one study[26] used the American Board of Orthodontics (ABO)[27] detailed objective classification system for models and radiographs which measures the details of a well-finished and well-balanced occlusion.
(Constructive criticism, however, is inherent in the statement itself: how is an efficient masticatory function and, therefore, a 'Normocclusion' defined?)
In Masticationpedia, we would like to launch interesting and constructive provocations to answer the question we just set out: 'How is an efficient chewing function and therefore a Normocclusion defined?'
Let's look at the two cases below, in figure 1 and in figure 2: which of the two clinical cases do you think is affected by malocclusion?
It seems irreverent for the canons of orthodox orthodoxy not to share the diagnosis of 'malocclusion', but we leave the reader in a little suspense. We intend to resume extensively in a few chapters, after deepening the topic of 'System Logic' and 'Systems Theory'. We only anticipate that the patient in figure 1 has already been proposed in the chapter 'Introduction', so we already know our clinical scientific opinion but if he gives us so much, also.....
(... be patient and you will see)
Medical language logic
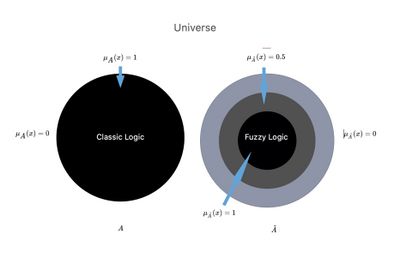
In the previous chapters we highlighted the extreme difficulties we met in defining an exact, detailed and timely diagnosis in the right time; and this is not only due to the 'Complexity' of the living system, but also to a questionable and vague logic of medical language. If classical logic is too selective (true or false, and therefore 'there is no third answer' - principle of the excluded third), it is also true that probabilistic logic language, which trivially indicates the presence of a specific disease, breaks down in the 'significativity' parameter that acquires a certain value only in a 'specialist context'.
We perceived the need for a more elastic model called "fuzzy logic" that could translate the uncertainty inherent in some human language data into mathematical formalism, codifying the "elastic" concepts (such as almost high, fairly good, etc), in order to make them understandable and manageable by computers.
We have therefore frozen a much debated and approached concept in the chapter 'Introduction': not determining a clear separation between specialist know-how, but superimposing interdisciplinary knowledge, instead, through a 'Fuzzy' approach (see fuzzy logic language).
Systems Theory
In the scientific field, systems theory, more properly general system theory (definition by Ludwig von Bertalanffy),[28] is an often interdisciplinary field of study, straddling mathematics and natural sciences, which deals with the analysis of properties and the constitution of a system. It is essentially composed of the theory of dynamic systems (simple and complex) and of the theory of control: it is the basis of various disciplines such as automation, robotics and cybernetic physics, as well as the technical-scientific study of systems in general as much as in biology and medicine.
Systems theory is the interdisciplinary study of systems, that could be described as cohesive groups of interconnected and interdependent parts that can be natural or man-made. Each system is bounded by space and time, influenced by its environment, defined by its structure and expressed through its functioning. A system can be more than the sum of its parts if it expresses emerging synergies or behaviors.[29]
Changing one part of a system might affect other parts or the whole system. It may be possible to predict these changes in behavior patterns. Some systems support other systems, keeping the others to prevent failure. The goals of systems theory are to model the dynamics, constraints, conditions of a system and to clarify the principles (such as purpose, measure, methods, tools) that can be identified and applied to other systems at any level of nesting and in a 'wide range of fields to achieve optimized equifinality.[30]
To be practical and effective in the description of the concept 'System logic' we consider an approach to a part of the trigeminal motor system, since it is the cornerstone of this scientific work, in which the conceptual connection with the 'Theory of Systems'.
Masticatory System Logic
Regarding the analysis of the state of the masticatory system, the EMG technique has been widely used but there are still a number of concerns regarding the reliability of the measures based on the interferential EMG.[31]
This is why most of the studies performed so far aimed at showing a possible correlation between EMG signals with Temporomandibular Disorders (TMD), Orofacial Pain (OP) or Malocclusion (IO), but they have not yielded convincing results.[32]
In an unknown percentage of OP patients visited by specialist dentists, some neurological diseases such as intracranial tumours, multiple sclerosis, etc. are the underlying symptoms cause of TMD or OP.
These patients, who actually suffer from neurological symptoms superimposed on dental-facial ones, may undergo unnecessary dental interventions before the correct diagnosis is made, sometimes too late.[33]
(... as said, the 'Observable' cannot be the occlusal element because it is hierarchically lower than the Trigeminal Nervous System.)
Cortical projections to the trigeminal motor neurons are generally believed to be bilateral and symmetrical and can be electrophysiologically analyzed by electrical or magnetic brain stimulation through the intact scalp.[34]
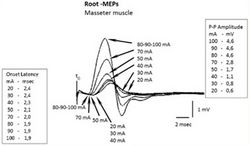
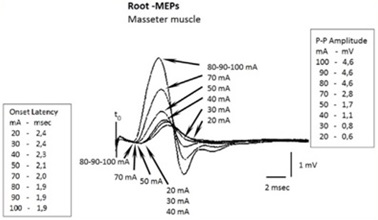
In the ipsilateral masseter, the transcranial electrical stimulation (eTCS) is capable of evoking a large short-latency potential in relaxed and active muscles. The characteristics of ipsilateral Motor Evoked Potentials (MEPs) do not change under relaxed or active conditions. Mean onset latency is approximately 2 ms, peak latency of 3.9 ms and amplitude of 5.4 mV, and there is no latency variability in similar pacing conditions. These motor potentials, considered secondary to trigeminal motor root excitation, have been called Root-MEP (Root-MEP or simplified into R-MEPs) to differentiate them from M-waves and Cortex-MEPs.[35]
To make the understanding of 'Systems Theory' more suitable for the context of the masticatory system, we report some trigeminal electrophysiological procedures and implement them with the mathematical models of the theory.
Mathematical formalism in 'Systems Theory'
The "systems theory" studies oriented systems, in which it becomes possible to classify the quantities of interest into two categories:
- quantities that vary over time independently from the others (inputs)
- quantities whose evolution over time is to be studied, depending on the inputs, called outputs.
A real system can have multiple inputs and multiple outputs. In particular, we indicate with:
- Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle u(t)= (u_1(t),..., u_r(t))} the vector of the inputs at time Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle {t}}
- Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle y(t)= (y_1(t),..., u_m(t))} the vector of the output at time Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle {t}}
It is also generally defined as the state vector of the system in a generic instant Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \tilde{t}} the information instantly Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \tilde{t}} necessary to uniquely determine the output Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle y(t)} for each Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle t\geq{\displaystyle {\tilde {t}}}} once the entrance has been assigned Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle u(t), } Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle t\geq{\displaystyle {\tilde {t}}}} .
We denote the state vector, whose components are defined as state variables, with the notation Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle x(t)= (x_1(t),..., x_n(t))} .
The inputs act on the state of the system and modify its characteristics at a given moment in time; these changes are recorded by the state variables. The values of the system outputs, usually the only measurable variables, in turn depend on the system state variables and the inputs.
The input, status and output quantities are functions of the time variable.
This takes values in an ordered subset Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle T \subseteq \R} , which can be continuous or discrete. In the following discussion we will consider a discrete subset of times:Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle T = \{t_0,..., t_s\}}
Therefore, given a set of times Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle T = \{t_0,..., t_s\}} , we can formally define a system as the pair of equations
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle x(t_{k+1})=f\bigl(x(t_k), u(t_k), t_k\bigr) }
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle y(t_k)=g\bigl(x(t_k), u(t_k), t_k\bigr) }
with Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle x(t_0)=x_0 } , where Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle f } is called generating function e Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle g } is called the output transformation.
In the field of biosignals, the (Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle g} ) models are used to analyze EEG and vibration systems in vehicles, human hearing systems and vascular systems, and so on. While much is still unknown about the physiological mechanism or pattern of internal changes in the tested system, the output transfer or transformation function Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle g} in our context allows us to reconstruct a wave function by interpolating the points detected by the instrument which has its own particular sampling frequency. This Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle g} function, for our purposes, is a reconstruction of a wave function on which to search for latencies, amplitudes and integral areas and make the necessary conclusions,[36][37] and, obviously, by retesting the system in subsequent epochs, the integrity of the system itself can be compared.
In the engineering field, various mathematical modeling of a system are possible, depending on whether or not they explicitly consider the state variables.
Mathematical formalism of the Trigeminal System Logic
We consider the Trigeminal Motor System as a black box with inputs (figure 5) and outputs (figure 6), and we try to adapt to it the above described theory.
Figure 6 shows the neuromotor responses to the electrical transcranial stimulation of the trigeminal root of the right hemilate. We wanted to set up the test following the mathematical model of 'systems theory' to better understand the difference between the information obtained from a now almost inflated test such as the interferential EMG, and a more complex test such as a motor and/or somatosensory evoked potential; the evoked potential has the prerogative of a system response to an external input called 'trigger', which in this context is of an electrical type.
We divided the test by delivering a series of progressively greater electrical stimuli in the ordered times corresponding toFailed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle T=\{t_0, t_1,t_2......t_{8}\}} .
In our context, we will have one input, i.e. the electrical stimulation amperage and two outputs, i.e. latency and amplitude.
We will therefore have:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \bigl(u(t_0), u(t_1), u(t_2), u(t_3), u(t_4), u(t_5), u(t_6), u(t_7), u(t_8)\bigr)=\bigl(0,20,30,40,50,70,80,90,100\bigr)} mA.
Two state variables will correspond to each of these inputs: latency Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \bigr( y_1(t) \bigl)} and amplitude Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \bigr( y_2(t) \bigl)} .
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \bigl(y_1(t_0), y_1(t_1), y_1(t_2), y_1(t_3), y_1(t_4), y_1(t_5), y_1(t_6), y_1(t_7), y_1(t_8)\bigr)=\bigl(0,2.4,2.4,2.3,2.1,2,1.9,1.9,1.9\bigr)} ms
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \bigl(y_2(t_0), y_2(t_1), y_2(t_2), y_2(t_3), y_2(t_4), y_2(t_5), y_2(t_6), y_2(t_7), y_2(t_8)\bigr)=\bigl(0,0.6,0.8,1.1,1.7,2.8,4.6,4.6,4.6\bigr)} mV
All these variables generate a plotting of multiple mediated traces as in figure 6, in which some important considerations can be made, such as the decrease in latency and the increase in amplitude as the amperage increases.
Conclusion
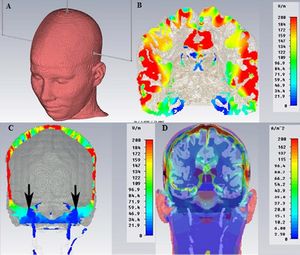
It is plausible that the reader, or a colleague not accustomed to particular trigeminal electrophysiological procedures, may consider this type of bioengineering diagnostic models exaggerated, both for the difficulty in the execution (that can make the methodology seem dangerous - the Root-MEPs delivers an electric current of 100 V with an amperage of 100mA), and for the feeling he might have that the cost benefit is unjustified; so, he might prefer to continue with the now routine methodology in dentistry, such as performing a simple, fast and inexpensive interferential EMG (Figure 7A). We certainly accept the opinion of our hypothetical colleague, but we do not share it because, to save a human life, competence is always and critically required, together with dedication and both intellectual and economic investment.
The irrefutable step forward made in diagnostics in most medical disciplines, as already mentioned, lies precisely in bioengineering, technological progress; specifically, systems theory has allowed us to verify the system state by comparing output variables generated by variables incoming payments which are basically triggers of various types.
Figure 7 is a way of demonstrating this. Notably, like the interferential EMG test shows (Figure 7A), only a sort of interferential asymmetry typical of clinical situations of malocclusion can be observed, while through a trigger model (specifically, the bilateral transcranial electrical stimulation of the trigeminal roots) the system responds with a large amplitude asymmetry (Figure 7B) and even with an absence of the jaw jerk response (evoked with a mechanical trigger by striking the chin with a neurological piezoelectric hammer). (Figure 7C) The diagnostic conclusion of this patient was of skull base menygoma.
For the experts, of course, a glance is enough to understand whether the trigeminal motor system evoked through electrical transcranial stimulation of the motor roots is in a physiological or pathological state; but, as we will see in the next chapters, the biological reality is so complex and paradoxically indeterministic, that a bioengineering model paired with an adequate statistical mathematician will allow us to approach more accurately the real physiopathological state of the system, reduce the uncertainty of the measurement and consequently the differential diagnostic error but above all make early diagnosis.
In any case, if this patient had undergone the described diagnostic model, he would not have died, because the growth of the tumor mass of a meningioma is extraencephalic, and slow, and would have shown an electrophysiologically documentable destructuring many years before the vertiginous symptomatology.(see: 3° Clinical case: Meningioma )
- ↑ Xiao W, Yang Y, Shi J, Xu J, Zhu J, «The diagnostic efficacy and predictive value of combined lipoprotein laboratory indexes for atherosclerosis», in J Pak Med Assoc, 2020».
PMID:33177739 - ↑ Ferraro D, Bedin R, Natali P, Franciotta D, Smolik K, Santangelo M, Immovilli P, Camera V, Vitetta F, Gastaldi M, Trenti T, Meletti S, Sola P, «Kappa Index versus CSF Oligoclonal Bands in Predicting Multiple Sclerosis and Infectious/Inflammatory CNS Disorders», in Diagnostics (Basel), MDPI, 2020».
PMID:33096861 - PMCID:PMC7589948
DOI:10.3390/diagnostics10100856
This is an Open Access resource! - ↑ Kayadibi H, Yilmaz B, Ozgur Yeniova A, Koseoglu H, Simsek Z, «Development and evaluation of a novel noninvasive index for predicting significant fibrosis, advanced fibrosis, and cirrhosis in patients with chronic hepatitis B infection», in Eur J Gastroenterol Hepatol., 2021».
PMID:33177385
DOI:10.1097/MEG.0000000000001973 - ↑ Results in PubMed for "Temporomandibular disorders Index"
- ↑ Results in PubMed for "Orthodontics Indexes"
- ↑ Sfondrini MF, Zampetti P, Luscher G, Gandini P, Gandía-Franco JL, Scribante A, «Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating)», in Healthcare (Basel), MDPI, 2020».
PMID:33182796 - PMCID:PMC7711869
DOI:10.3390/healthcare8040473.
This is an Open Access resource! - ↑ Dyken RA, Sadowsky PL, Hurst D, «Orthodontic outcomes assessment using the peer assessment rating index», in Angle Orthod, The EH Angle Education and Research Foundation, Inc., 2001».
PMID:11407767
DOI:<0164:OOAUTP>2.0.CO;2 10.1043/0003-3219(2001)071<0164:OOAUTP>2.0.CO;2 - ↑ 8.0 8.1 Richmond S, Shaw WC, O’Brien KD, Buchanan IB, Jones R, Stephens CD, Roberts CT, Andrews M, «The development of the PAR Index (Peer Assessment Rating): reliability and validity», in Eur J Orthod, Oxford University Press, 1992, Oxford UK».
PMID:1582457
DOI:10.1093/ejo/14.2.125 - ↑ Onyeaso CO, BeGole EA, «Associations between pretreatment age and treatment time with orthodontic treatment outcome: A comparison by means of two orthodontic indices», in Hell Orthod. Rev, MDPI, 2008, Basel, Switzerland».
- see alsoThis is an Open Access resource! - ↑ Hickman JH, «Directional edgewise orthodontic approach. 5», in J Clin Orthod, 1975».
PMID:1054697 - ↑ Firestone AR, Häsler RU, Ingervall B, «Treatment results in dental school orthodontic patients in 1983 and 1993», in Angle Orthod, The Edward H. Angle Society of Orthodontists, Inc., 1997, Bern, Switzerland».
PMID:10022180
DOI:<0019:TRIDSO>2.3.CO;2 10.1043/0003-3219(1999)069<0019:TRIDSO>2.3.CO;2 - ↑ Cook DR, Harris EF, Vaden JL, «Comparison of university and private-practice orthodontic treatment outcomes with the American Board of Orthodontics objective grading system», in Am J Orthod Dentofacial Orthop».
PMID:15953896
DOI:10.1016/j.ajodo.2004.12.014 - ↑ Ramanathan C, «PAR index in the evaluation of the stability of the orthodontic treatment results. A review», in Acta Medica (Hradec Králové), 2006, Hradec Králové, Czech Republic».
PMID:17438831
DOI:10.14712/18059694.2017.133 - ↑ Pangrazio-Kulbersh V, Kaczynski R, Shunock M, «Early treatment outcome assessed by the Peer Assessment Rating index», in Am J Orthod Dentofacial Orthop, 1999».
PMID:10229887
DOI:10.1016/s0889-5406(99)70277-5 - ↑ Templeton KM, Powell R, Moore MB, Williams AC, Sandy R, «Are the Peer Assessment Rating Index and the Index of Treatment Complexity, Outcome, and Need suitable measures for orthognathic outcomes?», in Eur J Orthod, Oxford University Press on behalf of the European Orthodontics Society, 2006, Oxford UK».
PMID:16648208
DOI:10.1093/ejo/cji120 - ↑ Angst C, Eliades T, Papageorgiou SN, «Stability of occlusal outcome during long-term retention: the time-dependent variation of the American Board of Orthodontics index», in Eur J Orthod, Zurich Open Repository and Archive, University of Zurich, 2021, Zurich, Switzerland».
PMID:32144422
DOI:10.1093/ejo/cjaa004 - ↑ Lyotard N, Hans M, Nelson S, Valiathan M, «Short-term postorthodontic changes in the absence of retention», in Angle Orthod, The EH Angle Education and Research Foundation, Inc., 2010».
PMID:20677953 - PMCID:PMC8929484
DOI:10.2319/010210-7.1 - ↑ Little RM, «Stability and relapse of dental arch alignment», in Br J Orthod., University of Washington, Seattle, 1990, Washington, USA».
PMID:2207055
DOI:10.1179/bjo.17.3.235 - ↑ Reitan K, Kvam E, «Comparative behavior of human and animal tissue during experimental tooth movement», in Angle Orthod, 1971».
PMID:4992550
DOI:<0001:CBOHAA>2.0.CO;2 10.1043/0003-3219(1971)041<0001:CBOHAA>2.0.CO;2 - ↑ Thilander B, «Dentoalveolar development in subjects with normal occlusion. A longitudinal study between the ages of 5 and 31 years», in Eur J Orthod, Oxford University Press on behalf of the European Orthodontic Society, 2009, Göteborg, Sweden».
PMID:19304760
DOI:10.1093/ejo/cjn124 - ↑ Behrents RG, Harris EF, Vaden JL, Williams RA, Kemp DH, «Relapse of orthodontic treatment results: growth as an etiologic factor», in J Charles H. Tweed Int Found, 1989».
PMID:2634695 - ↑ Lang G, Alfter G, Göz G, Lang GH, «Retention and stability--taking various treatment parameters into account», in J Orofac Orthop, 2002».
PMID:11974450
DOI:10.1007/s00056-002-0036-2 - ↑ Steinnes J, Johnsen G, Kerosuo H, «Stability of orthodontic treatment outcome in relation to retention status: An 8-year follow-up», in Am J Orthod Dentofacial Orthop, 2017».
PMID:28554448
DOI:10.1016/j.ajodo.2016.10.032 - ↑ de Freitas KM, Janson G, de Freitas MR, Pinzan A, Henriques JF, Pinzan-Vercelino CR, «Influence of the quality of the finished occlusion on postretention occlusal relapse», in Am J Orthod Dentofacial Orthop, 2007».
PMID:17920494
DOI:10.1016/j.ajodo.2007.02.051 - ↑ Hoybjerg AJ, Currier GF, Kadioglu O, «Evaluation of 3 retention protocols using the American Board of Orthodontics cast and radiograph evaluation», in Am J Orthod Dentofacial Orthop, 2013».
PMID:23810041
DOI:10.1016/j.ajodo.2013.02.022 - ↑ Nett BC, Huang GJ, «Long-term posttreatment changes measured by the American Board of Orthodontics objective grading system», in Am J Orthod Dentofacial Orthop, Elsevier Inc, 2005».
PMID:15821689
DOI:10.1016/j.ajodo.2004.03.029 - ↑ Casko JS, Vaden JL, Kokich VG, Damone J, James RD, Cangialosi TJ, Riolo ML, «Objective grading system for dental casts and panoramic radiographs», in Am J Orthod Dentofacial Orthop, 1998».
PMID:9810056
DOI:10.1016/s0889-5406(98)70179-9 - ↑ von Bertalanffy L, «General System Theory: Foundations, Development, Applications», in Arch Gen Psychiatry, George Braziller, 1968, New York».
ISBN: 978-0807604533
DOI:10.1001/archpsyc.1969.01740200123021 - ↑ Emergent Behaviour on PubMed
- ↑ Wikipedia article for Equifinality
- ↑ Reaz MB, Hussain MS, Mohd-Yasin F, «Techniques of EMG signal analysis: detection, processing, classification and applications (Correction)», in Biol Proced Online, 2006».
PMID:16799694 - PMCID:PMC1455479
DOI:10.1251/bpo115 - ↑ Masci C, Ciarrocchi I, Spadaro A, Necozione S, Marci MC, Monaco A, «Does orthodontic treatment provide a real functional improvement? A case control study», in BMC Oral Health, BioMed Central Ltd, 2013».
PMID:24152806 - PMCID:PMC3827987
DOI:10.1186/1472-6831-13-57
This is an Open Access resource! - ↑ Moazzam AA, Habibian M, «Patients appearing to dental professionals with orofacial pain arising from intracranial tumors: a literature review», in Oral Surg Oral Med Oral Pathol Oral Radiol, 2012».
PMID:23036798
DOI:10.1016/j.oooo.2012.06.017 - ↑ Merton PA, Morton HB, «Stimulation of the cerebral cortex in the intact human subject», in Nature, Springer Nature Limited, 1980».
PMID:7374773
DOI:10.1038/285227a0 - ↑ Cruccu G, Berardelli A, Inghilleri M, Manfredi M, «Functional organization of the trigeminal motor system in man. A neurophysiological study», in Brain, 1989».
PMID:2804615
DOI:10.1093/brain/112.5.1333 - ↑ Haebeom L, Hyunho K, Jungkuk K, Hwan-Sup O, Young-Jae P, Young-Bae P, «Feasibility study of transfer function model on electrocardiogram change caused by acupuncture», in BMC Complement Altern Med, 2017».
PMID:28178964 - PMCID:PMC5299648
DOI:10.1186/s12906-017-1615-5
This is an Open Access resource! - ↑ Smith RJ, Kamali G, Hays M, Coogan C, Crone NE, Kang JY, Sarma SV, «Transfer Function Models for the Localization of Seizure Onset Zone From Cortico-Cortical Evoked Potentials», in Front Neurol, Frontiers in Neurology, 2020».
PMID:33362689 - PMCID:PMC7758451
DOI:10.3389/fneur.2020.579961
This is an Open Access resource!
particularly focusing on the field of the neurophysiology of the masticatory system
Logic of Medical Language Diagnostic Model Masticatory Functions Quantum Mechanics Systems Theory Trigeminal Electrophysiological Analysis Bioengineering Technological Advances System State Diagnosis Motor Evoked Potentials Trigeminal Motor System Orthodontic Treatment Outcomes Diagnostic Indices Temporomandibular Disorders System Logic in Dentistry Clinical Model Accuracy