Jaw movements analysis. Part 1: Electrognathographic Replicator
Jaw movements analysis. Part 1: Electrognathographic Replicator
The Sirognathograph and related tools were once widely used to record mandibular movements for diagnosing TMDs. However, the RDC eliminated these devices, citing low validity in accurately diagnosing TMDs. Studies by Lund et al. demonstrated that such devices lacked sensitivity and specificity, often leading to false-positive diagnoses. Yet, their inability to capture complex rotational kinematics is due more to engineering limitations than inherent diagnostic flaws.
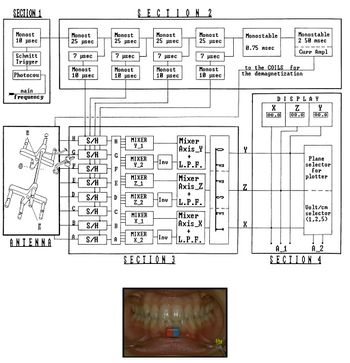
For instance, the Sirognathograph employs Hall effect sensors to capture linear displacements but fails to record angular rotations along critical axes like the sagittal and frontal planes. This loss of three angular degrees of freedom undermines its ability to fully represent the 6 degrees of freedom required for accurate mandibular modeling. Figure 1 illustrates this fundamental limitation.
Sampling Frequency: The Sirognathograph's sampling frequency of 50 Hz is insufficient for recording rapid or impulsive mandibular movements, such as those during a jaw jerk reflex or a meniscal click. As shown in prior research, the mandible’s displacement during these events occurs faster than the system's capacity to register. Modifying the device to increase the frequency to 500 Hz, as achieved in later prototypes, allowed the detection of mechanical latencies and improved spatial resolution of jaw movements (Figure 2).
Loss of Rotational Degrees of Freedom: The Sirognathograph only captures linear displacements along the X, Y, and Z axes but ignores the rotational components. During a mandibular opening or protrusion, simultaneous rotations and translations occur, especially at the working condyle. However, the mixing and inversion of sensor data suppresses angular information, leading to inaccuracies in reconstructing mandibular dynamics.
For instance, the angular displacement of 4.1° observed during mandibular opening is lost due to these engineering constraints. Without this data, clinicians cannot accurately calculate angular velocities, crucial for diagnosing specific TMDs or planning prosthetic rehabilitations.
Enhancing the Sirognathograph requires:: Increasing Sampling Frequency: Modifications to the circuit increased the sampling rate from 50 Hz to 500 Hz, improving temporal resolution for impulsive actions like the jaw jerk. Isolating Angular Data: Avoiding the summation and inversion of sensor outputs preserves angular displacements and allows better differentiation of rotational and translational movements. Redesigning Sensor Arrays: Positioning additional sensors along different axes could theoretically restore lost rotational degrees of freedom.
Clinical Implications: The loss of rotational data not only compromises diagnostic accuracy but also affects rehabilitative outcomes. For example:
Cuspal Errors in Prosthetics: Incorrect hinge axis localization due to missing angular data can result in errors in cusp alignment during prosthetic rehabilitation, affecting masticatory efficiency. Misdiagnosis of TMDs: The inability to differentiate between linear and angular displacements may lead to false positives in patients presenting with asymptomatic jaw deviations. However, the Sirognathograph's capacity to analyze linear displacements remains valuable for assessing orofacial pain in neurological disorders. Studies show alterations in mandibular kinematics in conditions like Parkinson's disease, where deviations in speed, trajectory, and rhythm of movement are prominent markers.
Conclusions: While the Sirognathograph is unsuitable for TMD diagnosis due to its engineering flaws, dismissing its potential in other clinical domains would be premature. Its application in differential diagnoses of neurological orofacial conditions remains promising. Future research should focus on redesigning diagnostic tools to better accommodate the complex kinematics of mandibular movements, ensuring precision in both diagnosis and treatment planning.
To read the full text of this chapter, log in or request an account
A Google Account is needeed to request a Member Account