Transcranial Magnetic Stimulation and Brain Plasticity in Post-Stroke Recovery
Transcranial Magnetic Stimulation and Brain Plasticity in Post-Stroke Recovery
Transcranial Magnetic Stimulation (TMS) is a completely harmless technique that allows specific areas of the brain to be stimulated.
By generating magnetic fields (1.5 - 2 tesla) of very short duration (< 1 msec) inside a toroid made of copper coils, and bringing the same close to the scalp, a very short-duration current is induced in the underlying brain, with the opposite direction to the current circulating in the toroid, without activating the nociceptors of the skin, muscles, or meninges.
This results in painless excitation of the neurons beneath the toroid. TMS allows mapping the connections of the motor system and defining its excitability.
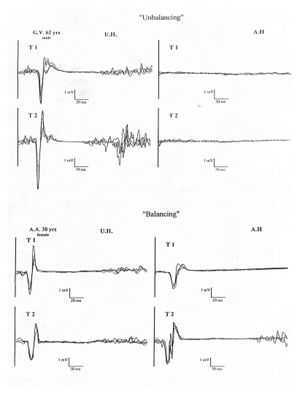
The evoked response can be derived from various muscles of the body, including those of the masticatory apparatus. In fact, stimulation of the scalp about 2 cm laterally to the central point of the scalp, identified as Cz according to the International 10-20 System of Jasper, evokes an electromyographic response recordable in the pterygoid and masseter muscles contralateral to the stimulated cortical area.
Multiple Motor Cortical Maps: Different body parts, such as the arm, leg, or face, have predominant representation in specific brain areas, but the representations of muscles of the same body part may overlap. In this respect, the motor cortex differs from the sensory cortex, which is organized in a simpler topography. For example, the cortical motor activity maps for the muscles that move different fingers are essentially the same, while in the sensory cortex, different fingers are represented separately, like the keys of a piano. Recent studies conducted at our center using TMS, stimulating the motor cortex and recording the motor response evoked from 12 muscles of the upper limb, have demonstrated that the neuron pools that govern various muscle groups have different excitability, accompanied by different scalp representation. Some muscles, in fact, showed a tendency to organize into “clusters,” aggregating into maps that widely overlapped each other, along with well-defined and separate hot-spot zones (point from which a motor response of minimum latency and maximum amplitude can be elicited) (Rossini and Pauri 2000, Fig.2).
This observation confirms the idea that the motor cortex is distributed over a network that extends across the entire strip of the classic M1 area of Brodmann, corroborating experimental data suggesting the existence of multiple motor cortical maps from both the primary and secondary motor and premotor cortices, with multiple topographically organized descending corticospinal pathways. Studies conducted with PET, fMRI, TMS, and EEG all agree on these basic concepts.
The pioneering studies by Merzenich and collaborators, conducted on monkeys, demonstrated that the organization of the sensory cortex changes after the transient or permanent loss of sensory information from a part of the body (e.g., a limb). Similar observations have been made by Donoghue and collaborators on the motor cortex. These studies showed that the cortex, no longer connected to the periphery, does not remain inactive but is “invaded” by the representation of body parts adjacent to the deafferented area, which had, in other words, been deprived of sensory information. Following reversible deafferentation, there is a temporary rearrangement of the somatotopic organization of the fingers in the primary somatosensory cortex, consisting of the expansion or displacement of cortical areas activated by the stimulation of unanesthetized fingers at the expense of cortical neurons deprived of sensory feedback.
Conclusions: The study results in stroke patients indicate that the affected hemisphere often undergoes significant remodelling of the sensory and motor somatotopy of the hand outside the usual control areas and/or an expansion of the hand representation area. The unaffected hemisphere, in turn, undergoes a reorganization process, albeit to a lesser extent. Ultimately, interhemispheric asymmetry appears to be the parameter with the highest sensitivity in describing brain reorganization following unilateral hemispheric injury. The importance of plastic phenomena in the recovery process highlights the importance of adequate physiotherapy. Taub and collaborators have advocated for the utility of resistance movement-based physiotherapy, forcing the use of hemiplegic limbs, even in chronic and apparently stabilized conditions. An expansion of the cortical map of muscles during the recovery phase has also been demonstrated in these patients. Even 6 years after a stroke, cortical motor output can be modified: with a “forced-use” paradigm, patients showed both an improvement in motor skill level and an enlargement of the motor representation area, while the cortical area related to the “healthy” limb, which was kept immobilized, contracted. Post-lesional recovery, as evidenced by the progressive normalization of cortical excitability, recovery of motor response amplitude, and latency, does not seem to be influenced by the rehabilitative method used, whether those using a peripheral-proprioceptive approach or those using a central-cognitive approach.
To read the full text of this chapter, log in or request an account
A Google Account is needeed to request a Member Account