Encrypted code: Bilateral Motor Evoked Potentials of trigeminal root
Encrypted code: Bilateral Motor Evoked Potentials of trigeminal root
Introduction
In the introductory chapter concerning the 3rd clinical case affected by meningioma in which the masticatory difficulty reported by the patient 'Balancer' had been correlated to a prosthetic rehabilitation discrepancy, we have already arrived at a first diagnostic filter considering the neurological assertion to be valid than the dental one. Consequently, one can concentrate on intercepting the tests necessary to decrypt the machine language code that the CNS sends out converted into verbal language. Apparently this verbal language would address the case in a Postural disorder related to a dental malocclusion due to incongruous prosthetic rehabilitation. If, on the one hand, there may be an asymmetry of the interferential EMG of the masseters due to a prosthetic occlusal imbalance, on the other, such an evident asymmetry of the jaw jerk and the silent period cannot be justified. For this reason, it is essential to continue with the Masticationpedia diagnostic model in order to arrive at an exact and rapid conclusive diagnosis. We therefore begin with the 'Cognitive Neural Network' which responds, as we know by now, with a sequence of scientific-clinical data, always taking into consideration the importance of the 'initiation' step which in this case has been set in 'Gait'.
Gait (45.300), motor evoked potentials (231),reflex (36), jaw(1) 'Cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS) with chronic cough and preserved muscle stretch reflexes: evidence for selective sparing of afferent Ia fibres'
Diagnostic sequence
1st Step: CNN Sequence
- Coherence Demarcator: As we have previously described for the other clinical cases, the first step is an initialization command of the Cognitive Neural Network 'CNN' which derives, in fact, from a previous cognitive elaboration on the assertions in the dental and neurological context in which the ' Demarcator of Consistency' gave a prevailing weight. The dental context has already been eliminated from the Consistency Demarcator. From what emerges from the neurological statements, the 'State' of the Trigeminal Nervous System' appears to be strongly damaged. The initialization command will therefore be 'Gait'.
- 1st loop open: The first result of the 'CNN' for the keyword 'Gait' returns 45,300 results, obviously, too vast to be exhaustive but having ascertained in the context analysis phase a serious trigeminal electrophysiological situation with marked structural anomalies and functional, we can safely enter a correlated key such as ' Motor Evoked Potentials' without specifying the trigeminal district which could encroach on the identified set.
- 2st loop open: To this second query 'Motor Evoked Potentials' the database replies with 231 results that are still too vast as an answer and therefore we are looking for a key more similar to the clinical case presented. Since the most anomalous results in the neurological context have emerged from the latency and amplitude alterations of the trigeminal reflexes, an appropriate access key could be, in fact, 'Reflex' also without specifying 'trigeminal' for the same anticipated reasons.
- 3st loop open: To the 'Reflex'request, the response was 36 results which narrowed the field of analysis for the diagnosis of our patient 'Balancer'. Only at this level of the CNN can one attempt to close the loop with a more specific request such as 'Jaw'. In this way we have not lost contact with the whole considered and we have remained in the field of electrophysiology.
- 4st loop open: The request 'jaw' in fact in the 36 results it is possible to intercept an article in which some electrophysiological parameters are reported which correspond to a clinical situation of cerebellar ataxia, a pathology in which postural and gait instability is a clinical sign impressive and important.
2st Step: CNN analysis
The 'CNN' loop closure analy of course is based on the terminal article which basically describe five patients with cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS) with chronic cough and lower limb muscle stretch reflexes preserve yourself.[1] In particular, somatosensory evoked potentials were absent or severely attenuated. Biceps and hamstring T-reflex recordings were normal, while the masseter reflex was absent or attenuated.
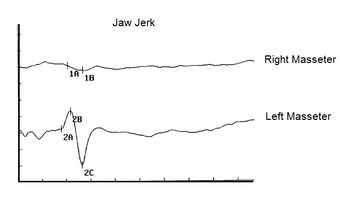
The first observation to be made is that the patients were suffering from chronic spasmodic cough and the second observation was the preservation of the tendon reflexes of the lower limbs. In our patient 'Balancer', on the other hand, there was a total absence of the mandibular tendon reflex[2] () so that the neurological damage was very evident at the trigeminal midbrain level. (Figure 1) The multifunctional contribution of the midbrain synaptic circuitry by the proprioceptive nerve endings ( e ) are of primary importance both for posture and for cervico-oculomotor reflexes. A very interesting article by Yongmei Chen et al.[3] showed, through markers, how neurons afferent to the trigeminal mesencephalic nucleus (Vme) from the jaw muscles project to the oculomotor nuclei (III/IV) and their premotor neurons in the interstitial nucleus of Cajal (INC), a well-known pre-oculomotor center that vertically manipulates torsional eye movements.
The conceptual conclusion of the authors was that the Vme proprioceptive neurons of the masticatory projecting muscles at III/IV and INC would detect spindle activity to spatial changes of the jaw conditioned by the force of gravity and/or by the connection between the mandible during rotation of the head. Thus, the convergent innervation of Vme and MVN neurons on the oculomotor and pre-oculomotor nuclei would be a neuroanatomical substrate for the interaction of masticatory proprioception with vestibulo-ocular signals on the oculomotor system during vertical-torsional VOR. The contribution of this article obviously allows us to consider a correlation between the trigeminal system, posture and gait, therefore, the abnormal asymmetry of the jaw jerk could be related to a postural disorder of our patient 'Balancer'
But there is also to consider the article of Jon Infante [1] highlighted that all five patients were in the seventh decade of age, their gait imbalance having started in the fifth decade. In four patients, cough preceded gait imbalance between 15 and 29 years of age; the cough was spasmodic and triggered by variable factors. In addition, vestibular function tests showed bilateral impairment of the vestibulo-ocular reflex.
The presence of chronic spasmodic cough, in this study, for over 10 years even before balance and postural disturbances showed up, suggest that machine language, as repeatedly exposed in the specific chapters of Masticationpedia, is a reality not to be overlooked because the ambiguous and vague verbal language covers the information of the encrypted code. As we will demonstrate in the course of the discussion, the analog of the spasmodic cough symptom of the patients reported by Jon Infante's article could be the repeated reporting to the dental colleagues of the chewing difficulty by our patient 'Balancer'. (Figure 2) This parameter has not been considered as an 'encrypted code' but only an element of verbal language logic and therefore vague and ambiguous. The continuous remaking of the prosthetic rehabilitation dampened even more the information of the machine language until the temporal and spatial addition of the organic damage was transformed[1] into a macroscopic symptom of vertigo and loss of balance in walking
Jon Infante's article[1] concludes with a striking statement, i.e. that spasmodic cough can be an integral part of the clinical picture in CANVAS, anticipating the appearance of postural imbalance by several decades and that sparing of muscle spindle afferents (Ia fibers) is probably the pathophysiological basis of normoreflexia.
(........is the neurological damage functional or organic?)
Decryption process
The diagnostic procedure followed routinely according to the Masticationpedia model has allowed us to eliminate, through the coherence demarcator, the dental context to follow the neurological one and to deepen through the 'Cognitive Neural Network' (CNN) the possible correlations between symptoms and neurophysiological abnormalities in patients with postural and walking disorders due to functional pathologies (labyrinthitis, neuropathies, etc.) from organic ones (tumors, demyelinations, etc.). Now we must try to decrypt the encrypted message of the machine language of the Trigeminal Nervous System.
Encrypted code
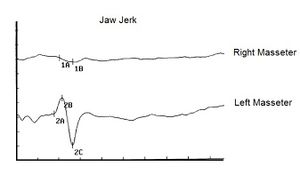
As anticipated, first of all we were able to highlight a serious absence of the jaw jerk reported as Abnormality, positive report (Figure 1) but as already mentioned in the chapter
' Conclusions on the status quo in the logic of medical language regarding the masticatory system' also in the patient treated with orthognathic surgery we were able to detect an absence of the jaw jerk (figure 2) restored immediately after evoked neurognathological rehabilitation. In our case 'Balancer' we have an additional objective disorder that of masticatory difficulty and together with the postural disorder there were nystagmus and vertigo.
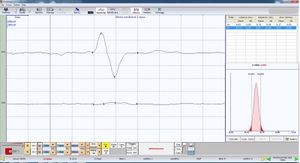
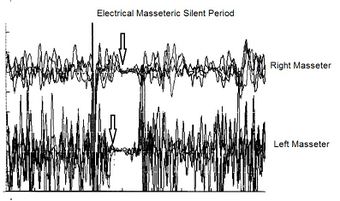
A further assertion in favor of organic damage was also the presence of a latency delay on the right side of the electrical silent period, Abnormality, positivity of the report, which suggests a slowing of the nerve conduction speed. In this instance we cannot say whether the delay refers to damage to the sensory or motor fibers until we approach the study of the nerve conduction of the motor trigeminal roots.
Motor evoked potentials of the trigeminal root
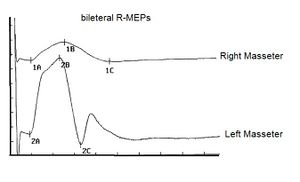
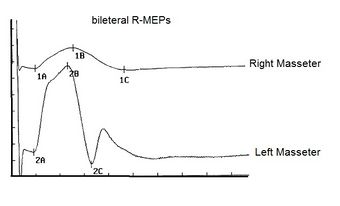
In our masticatory neurophysiology laboratory we have developed a technique of electrical transcranial electrostimulation of the two trigeminal roots simultaneously and synchronized with the electrical stimulus. In the various chapters already published some technical information on the method is reported but we intend to expose them exhaustively in the section 'Extraordinary science'. In this context we can only consider and confirm a significant amplitude asymmetry of the motor evoked responses as shown in figure 3. The markers 1A and 2A indicate the latency which, unlike the silent period, is symmetrical and this data confirms the structural damage of the sensory fibers including those proprioceptive from masticatory muscles. At this point we can not only confirm and justify the neurological choice of the diagnostic context but also conclude with a pre-diagnosis of cerebellar neurological damage with involvement of the trigeminal mesencephalic axis.
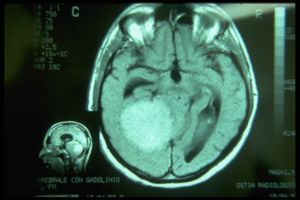
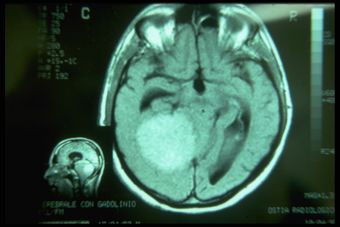
The Magnetic Resonance of the brain, unfortunately, solves our doubts with a report of solid expansive lesion with mass effect in the right hemisphere, it is not clear whether it has a supra or sub tentorial origin, it certainly determines compressive phenomena on the midbrain - trunk and on the fourth ventricle with dilatation of the cisternae and ventricles upstream. That it is a meningioma is very likely because he has no perilesional edema.
Final considerations
We summarize the clinical diagnostic path following the Masticationpedia model so that the latter can be considered a fluid and dynamic process to reach a diagnostic target in the fastest and most detailed way.
- Context analysis through dental and neurological laboratory tests
- Choice of neurological statement filtered by the Coherence Demarcator
- Evaluation of the clinical case in the Cognitive Neural Network (CNN)
- Closing the CNN loop with Jon Infante's article[1] and the consideration of the organic/functional damage of our patient's trigeminal sensory-motor structures through the observation of the amplitude asymmetry of the 'bRoot-MEPs'. The logical sequence of the tests carried out with the numbering restored has been ordered in the image gallery.
Conclusion
We now have evidence of both direct and indirect functional organic correlation between the trigeminal system and the vestibular system, just think of the study of mVEMP (Vestibular Evoked Myogenic Potentials) now recognized as a solid and reliable test for assessing the functional integrity of the reflex pathway vestibulo-masseteric[4] in clinical manifestations with involvement of the trigeminal and vestibular system as in schwannomas[5][6] or in the presence of acoustic neuromas[7] as much as the relative correlation between dental occlusion and the vestibular system but this does not allow, given the seriousness of the diagnostic error that it would result, to consider this last clinical condition a clinically validated scientific datum. In the Appendix an example of what might happen.
This last assertion, perhaps risky because it is controversial, collides with the evidence of a striking fact highlighted several times during the drafting of the chapters of Masticationpedia, that of machine language and verbal language. A vague and ambiguous verbal language can generate scientific convictions depending on how it is proposed but in substance it covers and hides a much more decisive and formal machine language. For example, the verbal language deduced that the postural disturbances of the 'Balancer' patient were caused by an incongruous prosthetic rehabilitation while the machine language signaled an organic sensorineural deficit (absence of the jaw jerk, latency delays of the silent period, large reduction in the amplitude of the bRoot-MEPs.
The lack of information on the velocity and the mandibular position at the midbrain level, in fact, determines an incapacity of stereognostic awareness in which the patient does not recognize the spatial and temporal position of the mandible. The decrease in the recruitment of the motor units of the masticatory muscles and not only of the tested masseter with an obvious decrease in the masticatory force is the result of this organic and functional damage. All this indicates an impairment of the proprioceptive territory but we do not know if the sensory structures have also been involved. The electrical silent period, on the other hand, shows a severe delay in latency with a slowing of nerve conduction velocity. To conclude the neurophysiopathological diagnostic picture is the observation that the right trigeminal motor root has lost most of its motor fibers.
However, it should be noted that in such a serious clinical condition we see a decrease in the amplitude of the bRoot-MEPs but not a latency asymmetry. This finding indicates that there was direct damage to the trigeminal motor fibers from tumor compression (axonotmesis) but not demyelination (neuropraxia) which would have shown latency delay on the right masseter. It is advisable to briefly describe the definition of neurological damage bearing in mind that the equivalent of the spinal peripheral nerve for the trigeminal nervous system corresponds to the motor trigeminal root.
Neurotmesis is caused by a transection of a nerve and is the worst degree of peripheral nerve injury. In neurotmesis, the entire nerve, including the endoneurium, perineurium, and epineurium, is completely severed. Neurotmesis leads to disruption of the axon, myelin sheath, and connective tissues. The prognosis for spontaneous recovery is poor without surgery.[8] Sunderland's fifth-degree lesion fits the definition of neurotmesis in the Seddon classification and represents the highest degree of nerve injury, with a complete nerve defect.
Neurapraxia is a nerve injury commonly induced by focal demyelination and/or ischemia and is the mildest type of peripheral nerve injury. In neurapraxia, nerve impulse conduction is blocked in the injured area, sensory and motor connection is lost, but all morphologic structures of the nerve stump, including the endoneurium, perineurium, and epineurium, remain intact.
Axonotmesis is a relatively more serious type of peripheral nerve injury and is usually caused by crushing, stretching, or percussion. In axonotmesis, the epineurium is intact, while the perineurium and endoneurium may be disrupted. The axon is separated from the soma and the axon and myelin sheath are disrupted. Wallerian degeneration occurs in the axon stump distal to the injury site within 24 to 36 hours after peripheral nerve injury.
After neurotmesis, Schwann cells respond adaptively to axonal disruption, transitioning from a highly myelinated state to a dedifferentiated state. De-differentiated Schwann cells engulf axons and myelin debris and form a regenerative pathway for axon outgrowth. Additionally, activated Schwann cells secrete a group of cytokines, including tumor necrosis factor-alpha, interleukin-1 alpha, and leukemia inhibitory factor, to recruit macrophages and facilitate digestion of debris. Schwann cells also secrete a group of neurotrophic factors, including nerve growth factor, brain-derived neurotrophic factor, and glial cell line-derived neurotrophic factor, to encourage neuron survival and axon elongation.[9][10][11]
Needle electromyography (EMG) is the most sensitive electrodiagnostic study for motor axon loss, and low-amplitude motor responses appear with severe injuries. Decrease in motor response amplitude begins around days 2-3 and is complete by day 6. This reflects the fact that neuromuscular junction degeneration precedes axon degeneration and motor responses are dependent on neuromuscular junction transmission.[12]
Appendix
Patient treated by a dental colleague for a prosthetic rehabilitation following postural methods which indicated the best Centric occlusion through dynamometric platforms. The patient came to our observation presenting a clinical state of fasciculation of the masseter muscles as well as, obviously, an occlusal and masticatory discomfort. The centric position finalized by the colleague was, therefore, correlated with the best postural dynamometry response but unfortunately this did not result.
Observing figures 5,6 and 7 we can understand how axioms are built that do not respond to a validated scientific criterion, much less to a biological reality. Thinking that a remote phenomenon such as postural stability dictated by a dynamometric platform can validate the choice of a position occlusal achieved manually by the operator breaks down on the observation that by observing the state of the trigeminal system by measuring it through a demand (bRoot-MEPs) the system responds with its own spatial position not dictated by posturological correlation nor by the manual maneuvers of the operator but by its own vectorial neuromotor result.
(….should only be considered as an experimental exploratory field to deduce more knowledge on neuronal connectivity.)
- ↑ 1.0 1.1 1.2 1.3 1.4 Jon Infante, Antonio García, Karla M Serrano-Cárdenas, Rocío González-Aguado, José Gazulla, Enrique M de Lucas, José Berciano. Cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS) with chronic cough and preserved muscle stretch reflexes: evidence for selective sparing of afferent Ia fibres.J Neurol . 2018 Jun;265(6):1454-1462. doi: 10.1007/s00415-018-8872-1.Epub 2018 Apr 25.
- ↑ Boes CJ. The history of examination of reflexes. .J Neurol. 2014 Dec;261(12):2264-74. doi: 10.1007/s00415-014-7326-7. Epub 2014 Apr 3.PMID: 24695995
- ↑ Chen Y, Gong X, Ibrahim SIA, Liang H, Zhang J.. Convergent innervations of mesencephalic trigeminal and vestibular nuclei neurons onto oculomotor and pre-oculomotor neurons-Tract tracing and triple labeling in rats. PLoS One. 2022 Nov 28;17(11):e0278205. doi: 10.1371/journal.pone.0278205. eCollection 2022.PMID: 36441755
- ↑ Sangu Srinivasan Vignesh, Niraj Kumar Singh, Krishna Rajalakshmi. Tone Burst Masseter Vestibular Evoked Myogenic Potentials: Normative Values and Test-Retest Reliability. J Am Acad Audiol. 2021 May;32(5):308-314. doi: 10.1055/s-0041-1728718.Epub 2021 Jun 1.
- ↑ Ashutosh Kumar, Sanjay Behari, Jayesh Sardhara, Prabhaker Mishra, Vivek Singh, Vandan Raiyani, Kamlesh Singh Bhaisora, Arun Kumar Srivastava . Quantitative assessment of brainstem distortion in vestibular schwannoma and its implication in occurrence of hydrocephalus.Br J Neurosurg . 2022 Dec;36(6):686-692. doi: 10.1080/02688697.2022.2047155.Epub 2022 Mar 7.
- ↑ Daniel Moualed, Jonathan Wong, Owen Thomas, Calvin Heal, Rukhtam Saqib, Cameron Choi, Simon Lloyd, Scott Rutherford, Emma Stapleton, Charlotte Hammerbeck-Ward, Omar Pathmanaban, Roger Laitt, Miriam Smith, Andrew Wallace, Mark Kellett, Gareth Evans, Andrew King, Simon Freeman. Prevalence and natural history of schwannomas in neurofibromatosis type 2 (NF2): the influence of pathogenic variants. Eur J Hum Genet. 2022 Apr;30(4):458-464. doi: 10.1038/s41431-021-01029-y.Epub 2022 Jan 24.
- ↑ Claudia Cassandro, Roberto Albera, Luca Debiasi, Andrea Albera, Ettore Cassandro, Alfonso Scarpa, Massimo Ralli. What factors influence treatment decision making in acoustic neuroma? Our experience on 103 cases. Int Tinnitus J. 2020 Nov 18;24(1):21-25.doi: 10.5935/0946-5448.20200004.
- ↑ Kaya Y, Sarikcioglu L. Sir Herbert Seddon (1903-1977) and his classification scheme for peripheral nerve injury. Childs Nerv Syst. 2015 Feb;31(2):177-80.
- ↑ Jessen KR, Mirsky R, Lloyd AC. Schwann Cells: Development and Role in Nerve Repair. Cold Spring Harb Perspect Biol. 2015 May 08;7(7):a020487.
- ↑ Madduri S, Gander B. Schwann cell delivery of neurotrophic factors for peripheral nerve regeneration. J Peripher Nerv Syst. 2010 Jun;15(2):93-103.
- ↑ Yi S, Zhang Y, Gu X, Huang L, Zhang K, Qian T, Gu X. Application of stem cells in peripheral nerve regeneration. Burns Trauma. 2020;8:tkaa002
- ↑ Ferrante MA. The Assessment and Management of Peripheral Nerve Trauma. Curr Treat Options Neurol. 2018 Jun 01;20(7):25.