'4° Clinical case: Temporomandibular disorders'
'4° Clinical case: Temporomandibular disorders'
Abstract
In the 'Introduction' chapter, we presented a demonstrative clinical case that challenged the concept of 'Malocclusion' in the sense that any class or occlusal morphology should always be related to trigeminal neuromotor responses to confirm the presence of a masticatory pathological disorder. In that case, the subject was found to have a perfect symmetry in latency, amplitude and integral areas of the trigeminal Central Nervous System (tCNS) and therefore hardly classifiable as 'malocclusion'. It should be borne in mind, however, that the subject in question with an obvious occlusal abnormality had absolutely no chewing disorder but what happens in a similar subject who reports orofacial pain and joint disorders. We will see in this chapter how such a patient should be considered and we will conclude with an exposition of the steps used for prosthetic rehabilitation performed with a trigeminal electrophysiological method called 'NGF model' which will be transformed, in the course of the Masticationpedia edition, into a diagnostic model called 'Index '
Introduction
An article by Ahmad and Schiffman[1] revealed interesting elements that call for a more in-depth analysis of the TMD phenomenon. The authors reported, in fact, that about 5-12% of the US population is affected by TMD and the annual cost of TMD management, excluding imaging costs, is about $4 billion. Interview Survey (NHIS) that included a total of 189,977 people, 4.6% (n = 8964) had temporomandibular joint and muscle disorders (TMJD).
As we have already mentioned several times in the previous chapters, one of the critical elements in the differential diagnosis between orofacial pain and TMD is the datum of the incidence of the disease, which necessarily pollutes the result of the predictive value of Bayes' theorem. In this case, from the authors' considerations[1] we are at 4.6 per cent.
We know by now that 'TMD' is the second most common chronic musculoskeletal condition after chronic low back pain[2] and although Ahmad and Schiffman[1] have exhaustively reported on the importance of imaging to make correct intra-articular diagnoses of TMJ, the doubt arises of the overlapping of symptomatic-clinical states as we have seen in the clinical cases reported in the previous chapters of Masticationpedia.
This interference does not depend on the physician's ability but on the deterministic forma mentis that leaves no room for the phenomenon of overlapping pathologies simulating the same TMD symptomatology. A quick roundup of clinical cases reported in the chapters of Masticationpedia can remind us better of the complexity and truthfulness of this statement. (Figure 1)
Rightly says Magda Krasińska-Mazur et al.[3] that the correct diagnosis of temporomandibular disorders is based on anamnesis and a thorough physical examination, as well as the results of additional tests.....but which ones?
(.... we will present in this context a diagnostic model in the context of restoring the functional masticatory condition of the patient in question)
So far we have discussed many aspects that in some way delay the differential diagnosis in patients who report overlapping symptomatology and various clinical manifestations, a differential diagnosis that if, on the other hand, performed correctly and quickly could save the subject's life as happened to our 'Bruxer' and unfortunately not to our 'Balancer'. The doctor's forma mentis in these cases is fundamental and the decisive element remains that of stepping out of the 'specialist context' in order to take an indeterministic and probabilistic view of medicine at the same time. This is no different with regard to patients actually suffering from TMDs because there is no real neuro-gnathological discipline, the diagnosis as well as the therapy of these subjects remains the standard one, namely gnathological. The discipline of gnathology, although very valid, is also limited because it restricts the field of the 'observable' to the occlusal parameter, disregarding everything else that is part of the masticatory neuromotor network and beyond.[4] We will present this clinical case of a patient with DTMs to give a significant clinical diagnostic/therapeutic change in the field of 'Functional Neuro Gnathology' calling it, precisely, the NGF method.
Anamnesis
As usual, we call our patient with a fancy name and precisely 'Clicker' because the patient had been suffering from temporomandibular joint (TMJ) clicks for years. Clicker presented to our neuropathology department complaining of severe orofacial pain and reporting a chronic right TMJ joint removal. She arrived after having already been diagnosed as DTMs always following the RDC protocol and treated with a biteplane to manage the nocturnal teeth grinding only. She, a 40-year-old patient who reported orofacial pain with joint noises such as clicks and crashes on both sides of the face and difficulty in chewing.
A first clinical occlusal examination shows a functional occlusal class III with sliding in protrusion in reaching the maximum intercuspidation. On palpation, the masseters, temporals, and external pterygoids on both sides were tender. No balance and gait disturbances, no vertigo, no tinnitus but as our routine we immediately performed trigeminal electrophysiological tests in order to avoid any structural involvement of the trigeminal Central Nevous System (tNCS). As already explained in the chapter concerning the 'Balancer' patient with Meningioma in which the interference EMG examination performed by the dental colleagues did not give indications of organic pathology of the tNCS in our Diagnostic Center we only perform Evoked Potentials and the battery of trigmeinal reflexes. In this chapter, taking into account the clinical situation, we have bypassed the purely dental context as, after an initial objective examination, the malocclusive disorder is striking but not certain (figure 2).
Trigeminal electrophysiology
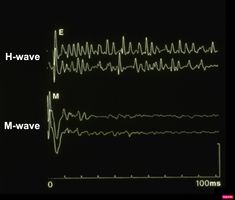
As has now been documented in the previous chapters of Masticationpedia, the heart of the scientific philosophy of Masticationpedia is substantially the normalization of masticatory functions to the Central Nervous System and trigeminal peripheral tCNS and not to dental occlusion. This is able to couple the occlusal abnormality to the 'state' conditions of the tCNS as well documented in the first chapter 'Introduction' where we showed a perfect trigeminal electrophysiological symmetry in the subject with severe dental malocclusion and a frankly asymmetric neuromotor condition in a subject with perfect occlusion after being treated with orthognathic surgery. The electrophysiological tests in subjects with TMDs are limited to the bilateral Motor Evoked Potentials of the trigeminal roots which we have precisely put over the years called bRoot-MEPs,[5] from the jaw jerk[6] performed while keeping the mandible in the rest position (Jaw jerk in rest position) and the jaw jerk keeping the jaw closed with moderate muscle activity (jaw jerk in occlusal position).
bRoot-MEPs
In figure 3 we can see the responses of the motor evoked potentials of the two trigeminal roots, the jaw jerk in the rest position and in the position of maximum intercuspidation. In particular, the Nervous system responds to Transcranial Electrical Stimulation of the trigeminal roots with two evoked potentials that are perfectly symmetrical both in latency and in amplitude and specifically the latencies are positioned at an onset of ms and ms while the peak-to-peak amplitudes mV and mV. This result is fundamental for the differential diagnosis between organic and functional pathologies, in fact, it demonstrates that the system is organically symmetrical and synchronous and this determines the term that we will see recur in a decisive way in the continuation of the Masticationpedia chapters called 'Organic Symmetry'. Bear in mind right now that the 'Organic Symmetry' parameter will be considered an element of 'Normalization' of the trigeminal reflex responses as its latency and amplitude symmetry indicates a perfect 'state' of integrity of the tCNS and that at the same time one should expect an equally 'state' of functional symmetry due to trigeminal reflex responses. Let's see, therefore, the trigeminal functional 'state' of the tCNS by analyzing the jaw jerk.
Jaw jerk in rest position
The stretch reflex test called jaw jerk was performed keeping the mandible in rest position to distinguish the input component to the tCNS excluding the input of the periodonatal receptors. The results were not encouraging due to the relative asymmetry of latency (ms and ms) and peak-to-peak amplitude (mV; mV). In particular, the latency delay could be explained by a facilitation on gamma motor neurons, in contrast with the study by Kitagawa et al.[7] in which it is asserted that the facilitation on the ipsilateral side could be produced by an enhancement of the gamma drive induced by a prolonged nociceptive stimulation. In our case the most significant datum is the difference of with reduction on the right affected side. We have noticed in our studies that in the rest position the jaw jerk also shows a dependence not only on the acceleration of the trigger stroke but also on the spatial position of the jaw as it is not conditioned by the occlusal position.[6]
Jaw jerk in rest position
The jaw jerk, keeping the mandible in a position of centric occlusion, performed to verify the contribution of the periodontal receptors together with the muscle and tendon proprioceptors, was obviously facilitated by the dental contact but the asymmetry in amplitude (mV; mV) increased. This result agrees with what was stated in a study by Yoshino T et al.[8] in which the mandibular position was deviated by 0.5, 1.0, 1.5, 2.0 and 3.0 mm to the right and left from a reference position corresponding to the rest position. Jaw jerk amplitude on the mediotrusive side increased primarily in proportion to mandibular deviation. The study concludes by suggesting that jaw jerk may aid the clinical examination of minor mandibular deviations. The conclusion of this 1st trigeminal electrophysiological step was to ascertain the organic integrity of the tCNS through the symmetry and synchronics of the bRoot-MEPs,[5] and consider it as an 'Organic Symmetry',[9] i.e. normalizer of the masticatory neurophysiological process while the asymmetries of the jaw jerk a functional disorder due to an unbalanced peripheral input or an inhibitory process on the trigeminal motoneurons of the nociceptive type. In essence, the conclusion of a mandibular spatial disorder would seem more indicative, which we will ascertain later when the Neuro Evoked Centric Relationship is performed to verify the physiological spatial position.
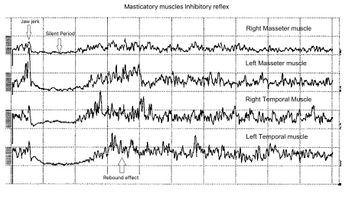
Silent period of the masticator muscles
Figure 4 shows the neuromuscular responses of the silent period to chin percussion through a triggered neurological hammer when the patient was asked to clench her teeth maximally. If from a neurological point of view it is not possible to highlight elements referable to organic alterations of the tCNS, some electrophysiological characteristics, however, are to be referred to a functional disorder of the system. In the upper trace, a decrease in the motor neuron reactivation phase can be seen immediately following the silent period. The possible neurophysiological mechanism capable of determining a similar decrease in facilitatory activities on the mandibular silent period can be ascribed to a change in the spindle motor drive induced by the input of muscle proprioceptors and nociceptors. The neuronal network of this process would take place through a loop formed by: muscle nociceptive afferents, the subnucleus caudalis of the V, inhibitory interneurons on static motor neurons and, as a last link, the modulation of the sensitivity of the neuromuscular spindles..[10] [11][12][13][14][15] Also in this context the inhibitory component most likely prevails over the excitatory one and this could be ascribed to a malocclusion as we will see later. In particular, it can be noted the overlapping of the jaw jerk behavior, previously tested, in a path rectification condition. The arrow indicates the jaw jerk on all traces and the decrease in amplitude can be observed for the right masseter while it is relatively symmetrical on the temporal muscles.
Mandibular spatial analysis
On this subject unfortunately there are innumerable conceptual conflicts redundant regularly coming back into vogue after a period of years such as the gothic arch tracing method to determine the centric relationship of full dentures, as suggested by Zhou TF et al.[16] From what has been exposed in all the chapters previously published on Masticationpedia, it is clear that the approximation of manual methods or vague interpretations derived from a logic of verbal language cannot be represented in the scientific philosophy of Masticationpedia which tends to focus on a mesoscopic model more than macroscopically descriptive and formal through statistical mathematical models as we will see below. Therefore we do not share the opinion of Zhou TF et al but absolutely in line with the concepts expressed by Silva Ulloa S. et al.[17] in which it is concluded that the sensorimotor cortex is affected by changes in occlusion and it is hypothesized that occlusion may play an important role in the development of diseases, from anxiety and stress to Alzheimer's disease and senile dementia. We also share the heartfelt suggestion of Silva Ulloa S. et al. in which she urges dentists to consider that alterations in the occlusal pattern during chewing can lead to changes in the activation of several brain regions related to memory, learning, anticipatory pain and anxiety.
(Relationship between dental occlusion and brain activity: A narrative review Sebastian Silva Ulloa, Ana Lucía Cordero Ordóñez, Vinicio Egidio Barzallo Sardi)
Therefore, it is essential to operate in synergy with the trigeminal neuromotor content in order to have an 'Observable' more indicative of the masticatory reality and in this case of the real spatial position that the jaw wants to reach beyond the dental interference. To achieve this target we have developed a method of simultaneous Transcranial Electrical Stimulation of the trigeminal roots which evokes a direct response of all the masticatory muscles which we call bRoot-MEPs as previously mentioned which has an indication of the 'state' integrity of the tCNS and at the same time it determines an elevation of the mandible from the rest position to the Occlusal Centric. This Centric has been named by us Functional Neuro Evoked Centric. (Figure 5)
As we can see, starting directly from a neurological context, using advanced trigeminal electrophysiological technologies, we have avoided the presence of destructuring of the tCNS and contextually highlighted a spatial-type occlusal disorder. The mandible with this method which generates a synchronous action potential of all the muscles innervated by the trigeminal roots, apart from conditions of marked destructuring of the ATM, generates a perfectly physiological closure which in this case is interrupted by the presence of a dental interference of the element 21 which comforts us in continuing the functional neurognathological treatment.
Functional Neuro Gnathological rehabilitation
Regarding the treatment of patients with TMDs there are still many strategic-conceptual conflicts such as, for example, the use of TENS[18] which the RDC protocol has considered clinically invalid as much as from a neurophysiological point of view TENS is not an appropriate method for not being able to evoke a response from all masticatory muscles but only the superficial ones. In this limitation lies the spatial error of the mandibular position which would be in a more anterior position due exclusively to the motor response of the masseter muscle (a topic which will be dealt with in the section 'Crisis of the Paradigm').
For this reason we bypass the manufacture of a bite plane to arrive directly at the definitive neurognathological prosthetic rehabilitation. In this specific case it was a Functional Neuro Evoked Centric rehabilitation of the anterior incisors and the four lower molars, two per side. The realization, however, followed some particularly obligatory pre-ordered steps which represent the best way to achieve real neuro-occlusal stability, as we will see in detail below. (figure 6)
In figure 6a we can see the structures of the crowns in the mouth on which the ceramic will be stratified and which will be covered with Aluvax wax to determine the Functional Neuro Evoked Centric. The decision to incorporate the four molars in the rehabilitation was made because these elements are crucial for occlusal stability but also for mediotrusion as we will see below. The exact mandibular position requires a third anterior point and for this reason, also considering the wear of the incisions and the importance of a normocclusion of the anterior sector, the involvement of the incisors was decisive for Centering the mandible in the optimal position (figure 6b) . Obviously, everything is brought back into articulate with mold waxes on Empress crowns. (figure 6c)
Functional Neuro Gnatologic Detail
For Neuro Gnatologic Functional detail, rehabilitation model called 'NGF Index' from which a whole scientific process will be initiated which will lead to a diagnostic paradigmatic model called 'NGF Index' in the 'Extraordinary Science' section, means an occlusal adjustment normalized to trigeminal neuromotor symmetry . To achieve this goal, gnathological replicates (articulated) and above all the ability to read the evoked and reflex responses of the tCNS in different occlusal situations are fundamental. For this reason, only the active centrics of the Empress crowns were stratified on the four lower molars. (figure 7)
In figure 7a, b and c only the active centrics of the molars have been stratified because although the Centric Neuro Evocate Functional registration is of absolute precision, the mechanical transfer from the mouth to the laboratory (articulator) could incorporate minimal spatial variations. For this reason it was decided to stop the neuro-evoked closure of the slightly raised jaw in order to have the availability of the ceramic material to be remodeled following the trigeminal electrophysiological responses. In essence, the cusps were abraded sectorally and individually to then compare with the trigeminal electrophysiological responses up to the perfect symmetry and synchronicity of the tCNS. Once the result of symmetry and synchronism has been achieved, the position reached will become the incisal rod at zero to conclude the stratification.
Figures 8a and 8b show the extraordinary differences in the trigeminal neuromotor response due, being of a functional type, to a mandibular spatial change and an accurate neurognathological occlusal balancing. In fact, one can see a symmetrization of the jaw jerk on the right masseter, a decrease in the duration of the mechanical silent period and above all an optimal motoneural reactivation after the silent period (rebound effect) which means safety in the total and immediate reactivation of the motoneural discharge. Once this trigeminal neuromotor re-symmetrization has been documented with irrefutable data, it is possible to move on to finalizing the clinical case.
NGF prosthetic rehabilitation
The finalization of the definitively diagnosed clinical case of DTMs resulted in a restoration of the masticatory function, disappearance of the symptoms as well as an aesthetic improvement. The various phases of the rehabilitation can be followed in the gallery of images in figure 9. In particular, the Functional Neuro-Evoked Centric position is not only centered having moved slightly to the right but also retruded. It is interesting to make a comparison with figure 5a to understand the spatial differences. Element 22, in fact, is no longer in crossbite but in a head-to-head position while element 23 has a much more incisal centric contact with respect to the previous clinical situation, so as to note the occlusal space in the medial area of element 24 which it was generated with the current mandibular spatial position determined with the Functional Neuro Evoked Centric. This new occlusal arrangement was only possible because the stable and mainly frozen centric position in the molar sector. The molars through the previously exposed neuromotor balance on the centric cusp stabilize the occlusion and generate a bilateral balance in the mandibular movements as will be shortly described.
In figure 9c and 9d, we can see not only the well balanced centric contacts but above all the mediotrusive excursions. A few more words should be spent on this subject. Benedikt Sagl et al.[19] state, in their study in which the contribution of tooth inclination, medio-otrusive and laterotrusive excursion and von Mises stresses on the articular disc was analysed, that mediotrusive bruxing generates higher loads than laterotrusive simulations. In this sense it is not clear whether the mediotrusive contacts are a protective or a pejorative element in the generation of temporomandibular joint disorders. So much so that an article by Walton TR and Layton DM[20] increases the confusion as they first state that the presence of TM interference in patient populations is large and varies from 0% to 77% and then conclude that TM interference should be avoided in any occlusal treatment regimen to minimize pulpal, periodontal, structural and mechanical complications or exacerbation of temporomandibular disorders (TMD). The confusion increases when he concludes that natural molar MT interferences should only be eliminated if signs and symptoms of TMD are present. The question that arises is the following
(.... are the interferences that cause the grinding and consequently damage to the atm or are the natural interferences protective on the system?)
It would be necessary to put some order on the subject starting with specifying what is meant by interference.
A study by Leitão AWA et al.[21] is extraordinarily significant having objectively simulated the interference in the animal and histologically analyzed the changes in the trigmeinal ganglion contextually with the behavior of the animal when treated with or without selective cyclooxygenase 2 (COX-2) inhibitor. Furthermore, the authors treated the animals with a daily infusion of 0.1 ml/kg of saline (DOI+SAL) and 16 or 32 mg/kg of celecoxib (DOI+cel -8, -16, -32 ). They noted that animals subjected to masseter nociceptive stimulation and interference DOI + SAL showed an increase in isplateral (P < 0.001) and contralateral (P < 0.001) nociception, an increase in the number of bites (P = 0.010), scratching (P < 0.001) and grimacing scores (P = 0.032) while in the DOI+cel-32 group, these parameters were reduced.
This interesting study shows the correlation between interference, decrease in pain threshold and contextually recovery with celecoxib infusion and therefore neuro-occlusal correlation.
Si-Yi Mo et al.[22] reinforces the above neuro-occlusal correlation by demonstrating that the descending pathway from serotonergic (5-HT) neurons in the rostral ventromedial medulla (RVM) to 5-HT3 receptors in the spinal trigeminal nucleus (Sp5), plays an important role in facilitating the maintenance of orofacial hyperalgesia after delayed removal of experimental occlusal interference (REOI).
Up to now we have a broader view on the subject of interference confirmed by the neuro-occlusal correlation but the phenomenon can also be seen locally in the articular disc. Another study by Cui SJ et al.[23] experimentally demonstrated that the effect of mechanical overload on TMJ discs in an in vivo rat occlusal interference model, inhibition of transient mechanoinductive receptor vanilloid potential 4 (TRPV4) alleviated TMJ disc degeneration in the rat occlusal interference model.
In conclusion, as we hope to share, the question is much more complex than what clinicians think and they hurry to eliminate the interferences, for example, mediotrusive because if the load induced on the joint, perhaps by a neuromotor hyperexcitability (see chapter Spasm Eimasticatorio and Cavernosa Pineale) the mediotrusive excursion could be a protective element perhaps to the detriment of the tooth itself.
For this reason, the term 'Mediotrusive Interference' should be re-evaluated
In figure 9c and 9d the mediotrusive path highlighted with the articulation paper was constructed by calculating the angle determined by the unilateral Root-MEPs which displaces the mandible by about 1/2mm on each side. By programming the Denar joint (figure 10) it was possible to construct an excursion with different angles between the TMJ, molar and canine. This procedure generates a natural path in which the canine guides together with the mediotrusion to protect the TMJ from the masticatory load that exists beyond bruxism.
Trigeminal Neuromotor Response, Malocclusion and TMD Diagnosis, Prosthetic Rehabilitation Techniques, Electrophysiological Methods in Dentistry, NGF Model in Masticatory Pathologies, Trigeminal Central Nervous System (tCNS), Dental Occlusion and Neuromotor Correlation, Masticatory Dysfunction Analysis, Index Psi Diagnostic Model, Clinical Case Studies in Dentistry,
- ↑ Jump up to: 1.0 1.1 1.2 Mansur Ahmad, Eric L Schiffman. Temporomandibular Joint Disorders and Orofacial Pain. Dent Clin North Am. 2016 Jan;60(1):105-24. doi: 10.1016/j.cden.2015.08.004.Epub 2015 Oct 21.
- ↑ Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and orofacial pain special interest group†. J Oral Facial Pain Headache 2014;28(1):6–27
- ↑ Magda Krasińska-Mazur, Paulina Homel, Andrzej Gala, Justyna Stradomska, Małgorzata Pihut. Differential diagnosis of temporomandibular disorders - a review of the literature.Folia Med Cracov. 2022;62(2):121-137. doi: 10.24425/fmc.2022.141703.
- ↑ Chiara Vompi, Emanuela Serritella, Gabriella Galluccio, Santino Pistella, Alessandro Segnalini, Luca Giannelli, Carlo Di Paolo. Evaluation of Vision in Gnathological and Orthodontic Patients with Temporomandibular Disorders: A Prospective Experimental Observational Cohort Study. J Int Soc Prev Community Dent PMID: 33042891 PMCID: PMC7523923 DOI: 10.4103/jispcd.JISPCD_273_19
- ↑ Jump up to: 5.0 5.1 Frisardi G. The use of transcranial stimulation in the fabrication of an occlusal splint.J Prosthet Dent. 1992 Aug;68(2):355-60. doi: 10.1016/0022-3913(92)90345-b.PMID: 1501190
- ↑ Jump up to: 6.0 6.1 Cruccu G, Frisardi G, van Steenberghe D. Side asymmetry of the jaw jerk in human craniomandibular dysfunction. Arch Oral Biol. 1992 Apr;37(4):257-62. doi: 10.1016/0003-9969(92)90047-c.PMID: 1520092
- ↑ Kitagawa Y, Enomoto S, Nakamura Y, Hashimoto K. Asymmetry in jaw-jerk reflex latency in craniomandibular dysfunction patients with unilateral masseter pain. J Oral Rehabil. 2000 Oct;27(10):902-10. doi: 10.1046/j.1365-2842.2000.00595.x.PMID: 11065026
- ↑ Yoshino T.Kokubyo Gakkai Zasshi. Effects of lateral mandibular deviation on masseter muscle activity. 1996 Mar;63(1):70-87. doi: 10.5357/koubyou.63.70.PMID: 8725358
- ↑ G Frisardi, G Chessa, A Lumbau, S Okkesim, B Akdemir, S Kara, F.Frisardi. The Reliability of the Bilateral Trigeminal Roots-motor Evoked Potentials as an Organic Normalization Factor: Symmetry or Not Symmetry. Dentistry S2 8, 2161-1122
- ↑ Ro J.Y.,Capra N.F.: Physiological evidence for caudal brainstem projections of jaw muscle spindle afferents.Exp.Brain Res 1999;128: 425-434
- ↑ Capra N.F.,Ro J.Y.: Experimental muscle pain produces central modulation of proprioceptive signals arising from jaw muscle spindles. Pain 2000; 86: 151-162.
- ↑ Appelberg B.,Hulliger M.,Johansson H.Sojka P.: Actions on g-motoneurones elicited by electrical stimulation of group III muscle afferent fibers in the hind limb of the cat.J Physiol. 1983;335: 275-292.
- ↑ Macefield G.,Hagbarth E,Gorman R, Gandevia SC,, Burke D.: Decline in spindle support to a-motoneurones during sustained voluntary contractions.J.Physiol 1991;440:497-512.
- ↑ Mense S.,Skeppar P.: Discharge behavior of feline gamma-motoneurones following induction of an artificial myositis.Pain 1991; 46: 201-210.
- ↑ Pedersen J, Ljubisavljevic M, Bergenheim M.,Johansson H.: Alterations in information trasmission in ensembles of primary muscle spindle afferents after muscle fatigue in heteronymous muscle.Neuroscience 1998;84: 953-959.
- ↑ Zhou TF, Yang X, Wang RJ, Cheng MX, Zhang H, Wei JQ.Beijing Da Xue Xue Bao Yi Xue Ban. A clinical application study of digital manufacturing simple intraoral Gothic arch-tracing device in determining the centric relation of complete dentures. 2023 Feb 18;55(1):101-107. doi: 10.19723/j.issn.1671-167X.2023.01.015.PMID: 36718696
- ↑ Silva Ulloa S, Cordero Ordóñez AL, Barzallo Sardi VE. Relationship between dental occlusion and brain activity: A narrative review. Saudi Dent J. 2022 Nov;34(7):538-543. doi 10.1016/j.sdentj.2022.09.001. Epub 2022 Sep 16.PMID: 36267531
- ↑ Didier HA, Cappellari AM, Gaffuri F, Curone M, Tullo V, Didier AH, Giannì AB, Bussone G. Predictive role of gnathological techniques for the treatment of persistent idiopathic facial pain (PIFP). Neurol Sci. 2020 Nov;41(11):3315-3319. doi: 10.1007/s10072-020-04456-9. Epub 2020 May 21.PMID: 32440980
- ↑ Sagl B, Schmid-Schwap M, Piehslinger E, Rausch-Fan X, Stavness I. The effect of tooth cusp morphology and grinding direction on TMJ loading during bruxism. Front Physiol. 2022 Sep 15;13:964930. doi: 10.3389/fphys.2022.964930. eCollection 2022.PMID: 36187792
- ↑ Walton TR, Layton DM. Mediotrusive Occlusal Contacts: Best Evidence Consensus Statement. J Prosthodont. 2021 Apr;30(S1):43-51. doi: 10.1111/jopr.13328.PMID: 33783093
- ↑ Leitão AWA, Borges MMF, Martins JOL, Coelho AA, Carlos ACAM, Alves APNN, Silva PGB, Sousa FB. Celecoxib in the treatment of orofacial pain and discomfort in rats subjected to a dental occlusal interference model. Acta Cir Bras. 2022 Aug 15;37(5):e370506. doi: 10.1590/acb370506. eCollection 2022.PMID: 35976283
- ↑ Mo SY, Xue Y, Li Y, Zhang YJ, Xu XX, Fu KY, Sessle BJ, Xie QF, Cao Y. Descending serotonergic modulation from rostral ventromedial medulla to spinal trigeminal nucleus is involved in experimental occlusal interference-induced chronic orofacial hyperalgesia. J Headache Pain. 2023 May 10;24(1):50. doi: 10.1186/s10194-023-01584-3.PMID: 37165344
- ↑ Cui SJ, Yang FJ, Wang XD, Mao ZB, Gu Y. Mechanical overload induces TMJ disc degeneration via TRPV4 activation. Oral Dis. 2023 Apr 27. doi: 10.1111/odi.14595. Online ahead of print.PMID: 37103670