Difference between revisions of "7° Klinischer Fall: Hirnstammneoplasie bei orofazialen Schmerzen"
| Line 33: | Line 33: | ||
<gallery widths="230" heights="200" perrow="3" slideshow""=""> | <gallery widths="230" heights="200" perrow="3" slideshow""=""> | ||
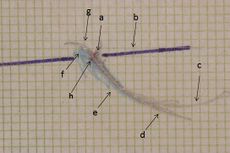
File:Assiografia dx modificata.jpeg|'''Abbildung 1:''' Rechtes konsuläres paraokklusales axiografisches Nachzeichnen: a) Zentrum der Scharnierachse, b) Orbitalebeneachse, c) prothetisches Nachzeichnen, d) medioprothetisches Nachzeichnen, e) medioprothetischer Kauzyklusbereich, f) lateroprothetischer Kauzyklusbereich, g) lateroprothetische Rücklinie, h) konsuläre Scharnierachse in maximaler Interkuspidation. | File:Assiografia dx modificata.jpeg|'''Abbildung 1:''' Rechtes konsuläres paraokklusales axiografisches Nachzeichnen: a) Zentrum der Scharnierachse, b) Orbitalebeneachse, c) prothetisches Nachzeichnen, d) medioprothetisches Nachzeichnen, e) medioprothetischer Kauzyklusbereich, f) lateroprothetischer Kauzyklusbereich, g) lateroprothetische Rücklinie, h) konsuläre Scharnierachse in maximaler Interkuspidation. | ||
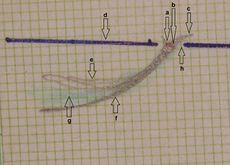
File:Assiografia sn.jpg| | File:Assiografia sn.jpg|'''Abbildung 2:''' Rechte konsulare paraokklusale axiografische Nachverfolgung: a) Scharnierachsenmitte, b) Orbitale Achsenebene, c) protrusive Nachverfolgung, d) mediotrusive Nachverfolgung, e) mediotrusiver Kieferzyklusbereich, f) laterotrusiver Kieferzyklusbereich, g) laterotrusive Rückenlinie. | ||
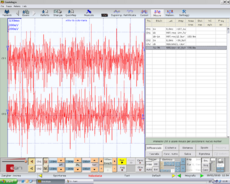
File:Frisardi Gianni 0001.bmp.png| | File:Frisardi Gianni 0001.bmp.png|'''Abbildung 2:''' Interferenzielle EMG der rechten (oben) und linken (unten) Masseter-Muskeln. Amplitude 200μV pro Teilung, Zeitteilung 100 msec. | ||
</gallery> | </gallery> | ||
</center> | </center> | ||
Der Satz {{:F:Imo}} (im zahnärztlichen Kontext) zusammen mit einer Anzahl <math>n\geq1</math> anderer logisch kompatibler Aussagen <math>(\delta_1,\delta_2,.....\delta_n \ )</math> bestimmen die Vereinigung und Kohärenz zwischen ihnen <math>\Im_o\cup\{\delta_1,\delta_2.....\delta_n\}</math> und werden mit einem mathematischen Formalismus dargestellt, um die diagnostische Dialektik auf folgende Weise <math>\Im_o\cup\{\delta_1,\delta_2.....\delta_n\}\rightarrow | |||
\Im_o\cup\{0,0.....0\}=0</math> | \Im_o\cup\{0,0.....0\}=0</math> zu erleichtern, was den Durchschnitt der einzelnen gemeldeten Behauptungen repräsentiert. Der Durchschnitt wurde gewählt, weil es häufig vorkommen kann, dass einige Tests negative Antworten liefern, denen der Wert <math>\delta_n=0</math> zugeordnet wird. Das Ergebnis ist in diesem Fall <math>\delta_n=0</math>, was kontextuell die kohärente Bestätigung des Satzes <math>\Im_o</math> ableitet, in dem argumentiert wird, dass die Symptomatik des 'Capsaicin'-Patienten nicht durch das Vorhandensein von TMDs bestimmt wird. | ||
In the ''neurological context'' we will therefore have the following sentences and assertions to which we obviously give, as for the dental context, a numerical value to facilitate the treatment and that is <math>\gamma_n=[0|1]</math> where i<math>\gamma_n=0</math> indicates 'normality' and <math>\gamma_n=1</math>'abnormality' and therefore positivity of the report: | In the ''neurological context'' we will therefore have the following sentences and assertions to which we obviously give, as for the dental context, a numerical value to facilitate the treatment and that is <math>\gamma_n=[0|1]</math> where i<math>\gamma_n=0</math> indicates 'normality' and <math>\gamma_n=1</math>'abnormality' and therefore positivity of the report: | ||
| Line 128: | Line 128: | ||
The interaction between neurons and immune cells is a well-known phenomenon.<ref>Jacobson A, Yang D, Vella M, Chiu IM (May 2021). "The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes". ''Mucosal Immunology''. '''14''' (3): 555–565. doi:10.1038/s41385-020-00368-1. PMC 8075967. <nowiki>PMID 33542493</nowiki>.</ref> TRPV1 plays its role, too, in neuroinflammation by being expressed in both neurons and immune cells. Significant importance should be given to the confirmed expression of TRPV1 in microglia and astrocytes, cells found in the vicinity of neurons. The neuro-immune axis is the site of production of neuroinflammatory molecules and receptors that interact between the two systems and ensure a complex response to external stimuli (or to the body's own pathologies). TRPV1 is said to contribute to microglia autophagy through its Ca<sup>2+</sup> signaling, which leads to mitochondria-induced cell death. Basically, TRPV1 is a pro-apoptotic element. | The interaction between neurons and immune cells is a well-known phenomenon.<ref>Jacobson A, Yang D, Vella M, Chiu IM (May 2021). "The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes". ''Mucosal Immunology''. '''14''' (3): 555–565. doi:10.1038/s41385-020-00368-1. PMC 8075967. <nowiki>PMID 33542493</nowiki>.</ref> TRPV1 plays its role, too, in neuroinflammation by being expressed in both neurons and immune cells. Significant importance should be given to the confirmed expression of TRPV1 in microglia and astrocytes, cells found in the vicinity of neurons. The neuro-immune axis is the site of production of neuroinflammatory molecules and receptors that interact between the two systems and ensure a complex response to external stimuli (or to the body's own pathologies). TRPV1 is said to contribute to microglia autophagy through its Ca<sup>2+</sup> signaling, which leads to mitochondria-induced cell death. Basically, TRPV1 is a pro-apoptotic element. | ||
===== Ligands===== | =====Ligands===== | ||
=====Antagonists===== | =====Antagonists===== | ||
Revision as of 19:11, 10 March 2024
7° Klinischer Fall: Hirnstammneoplasie bei orofazialen Schmerzen
Dieses Kapitel stellt einen Fall von absoluter epistemologischer Bedeutung dar, da es eine Lücke im diagnostischen Prozess aufzeigt, der auf evidenzbasierter Medizin (EBM) beruht. Dieser letzte Begriff ist tatsächlich untrennbar mit dem grundlegenden wissenschaftlichen Wissen verbunden, das bereits als Basiswissen bekannt ist.
Offensichtlich hängt dies vom wissenschaftlichen Fortschritt sowie von technologischer, methodologischer, aber auch philosophischer Entwicklung ab, da die Interpretation klinischer Daten in einem klassischen probabilistischen Modell die zugrunde liegende Realität nicht vollständig darstellen kann, da die Variablen abhängig und kompatibel sind, während sie in einem quantenmechanischen Modell unabhängig und inkompatibel sind. Dieser Paradigmenwechsel hätte es uns ermöglicht, detaillierte und frühzeitige Differentialdiagnosen zu stellen, ohne auf das Basiswissen zum spezifischen Thema Capsaicin bei Schmerzen warten zu müssen.
Dieses Kapitel war ein Meilenstein, der den Autor zur Schaffung von Masticationpedia führte, damit diese Fälle rechtzeitig erfasst werden können, um zumindest ein relativ friedliches Lebensende zu gewährleisten und nicht erst nach 10 Jahren Orofazialer Schmerzen (OP) durch Fehldiagnosen gesammelt werden müssen.
Einleitung
Der Hirnstamm ist der kaudale Teil des Gehirns, der das Zwischenhirn mit dem Rückenmark und dem Kleinhirn verbindet.[1] Der Hirnstamm vermittelt die sensorischen und motorischen Bahnen zwischen dem Rückenmark und dem Gehirn und enthält die Kerne der Hirnnerven, das aufsteigende retikuläre Aktivierungssystem (ARAS) und die autonomen Kerne. Er kontrolliert die Hirnstammreflexe und den Schlaf-Wach-Rhythmus und ist verantwortlich für die autonome Kontrolle des kardiovaskulären, respiratorischen, verdauungsmäßigen und immunologischen Systems. Eine Dysfunktion des Hirnstamms kann verschiedene akute oder chronische Schädigungen zur Folge haben, einschließlich Schlaganfall, Infektionen, Krebs, entzündliche und neurodegenerative Erkrankungen. Im Kontext schwerer Erkrankungen kann der Hirnstamm anfällig für verschiedene Schädigungen sein, die als struktureller und nicht-struktureller Ursprung klassifiziert werden können. Eine Hirnstammdysfunktion kann daher zu einer Beeinträchtigung des Bewusstseins, der kardiovaskulären und respiratorischen Insuffizienz und somit zu einer erhöhten Sterblichkeit beitragen[2][3][4][5] und sich insbesondere als Orofazialschmerz (OP) manifestieren. Hirnstammdysfunktion bei kritisch kranken Patienten:Brainstem dysfunction in critically ill patients:
Diese wichtigen Voraussetzungen, die aus einem interessanten Artikel von Sarah Benghanem[6] extrahiert wurden, sind wesentliche Details, die Ausdruck einer klinischen Erfahrung sind, die den Autor des Kapitels zu wissenschaftlichen und epistemologischen Überlegungen über die Art der Sprache geführt hat, die bei der Erstellung von Diagnosemodellen verwendet werden soll, und folglich zur Gründung von Masticationpedia geführt hat. Man kann nicht, wie es die persönliche und verantwortungsbewusste Aussage des Autors der Kapitel zeigt, sklavisch einem Axiom oder einem Protokoll wie dem DRC oder ähnlichem folgen und das Risiko eines Differentialdiagnosefehlers eingehen, der das Leben eines Menschen kosten kann. Wenn es eine Lücke im Modell gibt, die wir während der Implementierung von Masticationpedia nachweisen werden, dann sollte sie als Anomalie vermerkt, analysiert und beseitigt oder zumindest modifiziert werden, sonst handelt es sich nicht um paradigmatischen Fortschritt, sondern nur um intensiven Fortschritt.
Vorstellung des klinischen Falls
Es war das Jahr 1995, als die 60-jährige Patientin, die wir mit einem ausgefallenen Namen "Capsaicin" nennen werden (den Grund werden wir unten verstehen), sich mit bilateralen diffusen Orofazialschmerzen in der Region der Schläfenmuskulatur und im okzipitalen Bereich, zusätzlich zum Vorhandensein von brennendem Mund (BMS), seit mehr als 10 Jahren bei uns vorstellte. Die Schmerzen dauerten stundenlang, besonders nachts, und traten nicht zyklisch auf. Die Patientin trug seit langem eine obere und untere keramische feste Prothesenrehabilitation mit verschiedenen Brüchen der keramischen Struktur und Abrieb-Veneers auf den verbleibenden natürlichen Zähnen. Es wurden jedoch keine Okklusionsdiskrepanzen in der prothetischen Rehabilitation festgestellt, sondern von anderen Gesundheitsfachkräften wurde eine Entlastungsplatte zur nächtlichen Anwendung angefertigt. Die Patientin berichtete auch bei eingelegter Platte über Schmerzen und wurde zunächst als von Atypischen Orofazialen Schmerzen (AOP) mit einem starken psychosomatischen Komponenten betroffen betrachtet und später, gemäß dem RDC-Protokoll, als von 'Temporomandibulären Störungen' betroffen.
Nach unserer Untersuchung, gemäß dem Masticationpedia-Protokoll, wurden die wichtigsten gnathologischen Tests durchgeführt, wie paraokklusale Axigraphie der kondylären Spuren und eine interferenzielle EMG der Massetermuskulatur. In diesem Fall wurde kein ATM-CT angefordert, geschweige denn ein MR. Wir stellen schematisch und repräsentativ einige Absätze aus den vorherigen Kapiteln dar, die das Masticationpedia-Protokoll in seiner Schematisierung als: Aussagen im zahnärztlichen, neurologischen Kontext und schließlich die diagnostische Schlussfolgerung durch den 'Demarcator' vorstellen ':
Bedeutung von Kontexten
Für den "zahnmedizinischen Kontext" haben wir die folgenden Sätze und Aussagen, denen wir einen numerischen Wert zuordnen, um die Behandlung zu erleichtern, und das ist wobei 'Normalität' anzeigt und 'Abnormalität und somit Positivität des Berichts' bedeutet:
Paraokklusales axiografisches Nachzeichnen des rechten Kondylus, negativ in Abbildung 1, Normalität, negativer Bericht
Paraokklusales Axiografie-Nachzeichnen des linken Kondylus, negativ in Abbildung 2, Normalität, negativer Bericht
Symmetrisches EMG-Interferenzmuster in Abbildung 5. Normalität, negativer Bericht
Abbildung 1: Rechtes konsuläres paraokklusales axiografisches Nachzeichnen: a) Zentrum der Scharnierachse, b) Orbitalebeneachse, c) prothetisches Nachzeichnen, d) medioprothetisches Nachzeichnen, e) medioprothetischer Kauzyklusbereich, f) lateroprothetischer Kauzyklusbereich, g) lateroprothetische Rücklinie, h) konsuläre Scharnierachse in maximaler Interkuspidation.
Der Satz (im zahnärztlichen Kontext) zusammen mit einer Anzahl anderer logisch kompatibler Aussagen bestimmen die Vereinigung und Kohärenz zwischen ihnen und werden mit einem mathematischen Formalismus dargestellt, um die diagnostische Dialektik auf folgende Weise zu erleichtern, was den Durchschnitt der einzelnen gemeldeten Behauptungen repräsentiert. Der Durchschnitt wurde gewählt, weil es häufig vorkommen kann, dass einige Tests negative Antworten liefern, denen der Wert zugeordnet wird. Das Ergebnis ist in diesem Fall , was kontextuell die kohärente Bestätigung des Satzes ableitet, in dem argumentiert wird, dass die Symptomatik des 'Capsaicin'-Patienten nicht durch das Vorhandensein von TMDs bestimmt wird.
In the neurological context we will therefore have the following sentences and assertions to which we obviously give, as for the dental context, a numerical value to facilitate the treatment and that is where i indicates 'normality' and 'abnormality' and therefore positivity of the report:
bRoot-MEPs symmetrical in amplitude and latency in Figure 4, Normality, negative report
Jaw jerk symmetrical in amplitude and in latency in Figure 8, Normality, negative report
Symmetry in duration of the masseter silent period in Figure 6, Normality, negative report
Consequently even in sentence with a number of other logically compatible assertions they determine the union and coherence between them and the formal representation will be similar to that of the dental context. with contextual coherent affirmation of the sentence in which it is argued that the symptomatology of the patient 'Capsiacin' does not electrophysiologically highlight any element that could indicate a correlation between orofacial pain and neuromotor damage.
Coherence Demarcator
The is a representative clinical specific weight, complex to research and develop because it varies from discipline to discipline and for pathologies, essential for not colliding logical assertions and in diagnostic procedures and fundamental for initializing the decryption of the machine code. Basically it allows to confirm the coherence of one union with respect to another and vice versa, giving greater weight to the seriousness of the assertions and of the report in the appropriate context. Sometimes the doctor is faced with a series of positive reports to which he must give the right weight, he must consider the positivity of a report which highlights, for example, an osteoarticular renewal of the TMJ cannot have the same weight as a positivity of a report confirming latency delay of a trigeminal reflex. The demarcation weight, therefore, gives more significance to the more serious assertions in the clinical context from which they derive and therefore beyond the positivity of the assertions or which in any case are always verified and respected, these must be multiplied by a where indicates 'Low seriousness ' while 'Severe Gravity'.
A consistency marker could be defined as a real number between 0 and 1 in the event that we have more than two reports and therefore a number close to zero would correspond to a report of 'low severity' while a number close to one to a reporting of 'severe severity'. But this is redundant. What is done is to compare the reports two by two and then use the values we have indicated to express the 'Gravity'.
So to recap we have:
where
average of the value of the clinical statements in the dental context which in our case in question is
average of the value of clinical statements in the neurological context and therefore
reporting of low severity of the dental context
reporting of low severity of the neurological context
where the 'demarcator of coherence marker' will define the diagnostic path as follows
As we will see during the exposition of the clinical cases in Masticationpeida, one will be faced with similar clinical situations in which you are in the presence of orofacial pain but the reporting results in specialist contexts will be of low severity such as to cancel the discriminate value of .
(The fact remains that the patient continues to experience orofacial pain and particularly with exacerbation after a spicy dinner.)
In the rare but real clinical cases in which the ' Demarcator' is reset, we are motivated to carry out an even more extensive and in-depth check, hypothesizing serious pathologies [7][8] including head and neck tumors which simulate symptoms that can be superimposed on other pathologies. It is a serious mistake to consider the patient with such clinical manifestations and the simultaneous absence of systemic anomalies as a patient with psychosomatic disorders. Elements of psychophysical damage can certainly coexist but, if the 'Demarcator' fails, it is mandatory to deepen the diagnostics. In fact, head and neck cancer (HNC) affects over 890,000 people each year worldwide and has a 50% mortality rate. Aside from poor survival, HNC pain impairs eating, drinking and speaking, severely reducing quality of life. The different pain phenotype in patients (allodynia, hyperalgesia, and spontaneous pain) results from a combination of anatomical, histopathological, and molecular differences between tumors[9]. Glial and immune modulation of the tumor microenvironment, as well explained in the article by Ye et al., influences not only cancer progression but also pain signaling among which transient receptor potentials contained in gustatory somatosensory systems are an example.[10][11]
For the above reasons and for the persistence of the OP, the difficulty in concluding a certain diagnosis, the absence of organic-functional discrepancies and the zeroing of the ' Demarcator', an MR of the brain was requested.
Imaging showed a neoplastic mass most likely a brainstem schwannoma with invagination of the occipital frame. (figure 7 and 8)
(.......leaving a doubt, that of the correlation between pain and capsaicin as reported by the patient on the occasion of a spicy diet.)
Thoughts and conclusions
The mammalian gustatory system is made up of taste buds, which are clusters of 50-100 taste cells found throughout the oral cavity. On the tongue, which is the central topic of the case report 'Capsaicin', the taste buds are located on circumvallate, foliate and fungiform papillae. Taste cells synapse with afferent fibers from branches of the cranial facial (CN VII), glossopharyngeal (CN IX) and vagus (CN X) nerves which, in turn, transmit information to the central nervous system (CNS) about gustatory attributes , intensity and hedonic nature. [12][13][14] The taste buds are embedded in a stratified squamous epithelium, which contains somatosensory branches of the trigeminal (CN V), glossopharyngeal (CN IX), and vagus (CN X) cranial nerves. Information from these general sensory nerves provides information to the central nervous system about mechanical, thermal, and pain stimuli.[11][15] Painful stimuli can result from strong or sharp mechanical stimuli, abnormally high or low temperatures, or chemical stimuli such as capsaicin, which is found in hot peppers and causes a burning taste sensation through the intervention of Transient Receptor Potentials (TRPs).[10] These TRPs are divided into six subfamilies including TRPV1, which we are interested in to hypothesize the phenomenon of pain exacerbation of the patient 'Capsaicin' in spicy diet.

TRPV1 and neuroinflammation
TRPV1s constitute a distinct subset of non-selective cation channels (Transient Receptor Potential) responsible for many cellular responses. They are activated by various stimuli such as acids, extracellular protons, high temperatures, plant toxins and vanilloid agonists. The TRPV1s present in mammals can be considered as sensors of chemical substances (capsaicin), thermal substances (heat) and/or harmful stimuli. The activation of TRPV1 leads to the depolarization necessary for the propagation of action potentials along the axons of the dorsal root ganglia (DRG) of neurons that project to the spinal cord and consequently also to the nociceptive trigeminal nuclei. What makes TRPV1 so critical for pain signaling is undeniably its ability to transduce inflammatory signals into electrical signals with the activation of both voltage-gated sodium and calcium channels located at the nociceptor level.[16] The implication of TRPV1 in pathological pain prompted a careful study of these proteins. The limiting element in pharmacological research at the application level was the peculiarity of the TRPV1 channel, i.e. its polymodal mechanism of activation (heat, capsaicin, pH), which led to a high level of complexity in the design of a specific modality inhibitor.
The interaction between neurons and immune cells is a well-known phenomenon.[17] TRPV1 plays its role, too, in neuroinflammation by being expressed in both neurons and immune cells. Significant importance should be given to the confirmed expression of TRPV1 in microglia and astrocytes, cells found in the vicinity of neurons. The neuro-immune axis is the site of production of neuroinflammatory molecules and receptors that interact between the two systems and ensure a complex response to external stimuli (or to the body's own pathologies). TRPV1 is said to contribute to microglia autophagy through its Ca2+ signaling, which leads to mitochondria-induced cell death. Basically, TRPV1 is a pro-apoptotic element.
Ligands
Antagonists
Antagonists block the activity of TRPV1, thereby reducing pain. Antagonists identified include the competitive antagonist capsazepine and the non-competitive antagonist ruthenium red. These agents could be beneficial if applied systematically.[18] TRPV1 antagonists have shown efficacy in reducing nociception from inflammatory and neuropathic pain models in rats.[19] This provides evidence that TRPV1 is the sole receptor for capsaicin.[20] In humans, drugs that target TRPV1 receptors could be used to treat neuropathic pain associated with multiple sclerosis, chemotherapy, or amputation, as well as pain associated with the inflammatory response of damaged tissue, such as in osteoarthritis.[21]
Agonists
TRPV1 is activated by several agonists of natural origin.[22] Agonists such as capsaicin and resiniferatoxin activate TRPV1 and, after prolonged application, cause the decrease of TRPV1 activity (desensitization), leading to pain relief through the subsequent decrease of the TRPV1-mediated release of inflammatory molecules upon exposure to noxious stimuli.
An interesting study by the Tominaga group extends the list of TRPV1 interactions also to Anoctamin 1 (ANO 1) also known as Transmembrane member 16A (TMEM16A) a chloride channel which is usually activated by Ca2+. The authors demonstrate, in fact, that when TRPV1 interacts with the ANO1 channel it mediates the efflux of Chloride evoking depolarization (after stimulation by capsaicin) with increased excitability of the nociceptor. Tominaga highlighted a clear structural and functional crosstalk between TRPV1 and ANO1, which intervenes in the algogenic action of capsaicin.
These results demonstrate the importance of chloride homeostasis in the regulation of the excitability of the neuronal DRGs, i.e. of the dorsal root ganglia and obviously of the trigeminal somatosensory nuclei and in the pain phenomenon as a whole; one of the new approaches, therefore, where to intervene to mitigate painful hypersensitivity and neurogenic inflammation.
TRPV1 is activated by several agonists of natural origin. Agonists such as capsaicin and resiniferatoxin activate TRPV1 and, after prolonged application, cause the decrease of TRPV1 activity (desensitization), leading to pain relief through the subsequent decrease of TRPV1-mediated release of inflammatory molecules following administration. exposure to noxious stimuli.
An interesting study by the Tominaga group extends the list of TRPV1 interactions also to Anoctamin 1 (ANO 1) also known as Transmembrane member 16A (TMEM16A)[23] a chloride channel which is usually activated by Ca2+. The authors demonstrate, in fact, that when TRPV1 interacts with the ANO1 channel it mediates the efflux of Chloride evoking depolarization (after stimulation by capsaicin) with increased excitability of the nociceptor. Tominaga[23] highlighted a clear structural and functional crosstalk between TRPV1 and ANO1, which intervenes in the algogenic action of capsaicin.
These results demonstrate the importance of chloride homeostasis in the regulation of the excitability of the neuronal DRGs, i.e. of the dorsal root ganglia and obviously of the trigeminal somatosensory nuclei and in the pain phenomenon as a whole; one of the new approaches, therefore, where to intervene to mitigate painful hypersensitivity and neurogenic inflammation.
(....for chronic damage to the brainstem nerve fibers with consequent alteration of the neuro-immune homeostasis and contextual paradoxical effect of the analgesic action of capsaicin.)
In these cases, as stated in other chapters, we are dealing with an epistemological profile in which the basic knowledge, what we have called (Knowledge Base) corresponds to a temporal limit of scientific information and consequently serious difficulties of differential diagnosis. We had to wait 12 years to reach an ezipathogenetic conclusion overwritten from 1995, a period in which the patient 'Capsaicin' was being treated, to 2007 in which a research gave the elements to suspect the presence of an organic neurological damage with manifestations of pain and burning mouth.[24] Burning mouth syndrome (BMS) is often an idiopathic, chronic intractable pain condition, affecting 1.5-5.5% of middle-aged and older women. We investigated heat and capsaicin receptor TRPV1, and its regulatory nerve growth factor (NGF), in BMS. BMS patients (n=10) and controls (n=10) were evaluated for baseline and post-topical capsaicin pain scores, and their tongue biopsies were immunostained for TRPV1, NGF, and neurofilament structural nerve markers and periphery. Nerve fibers penetrating the epithelium were less abundant in the BMS (p<0.0001), indicating small fiber neuropathy. TRPV1-positive fibers were overall significantly increased in BMS (p=0.0011), as were NGF fibers (p<0.0001) and NGF staining of basal epithelial cells (p<0.0147). There was a significant correlation between baseline pain score and TRPV1 (p=0.0143) and NGF (p=0.0252) fibers. A significant correlation was observed between baseline and post-capsaicin pain (p=0.0006).
- ↑ Hurley RA, Flashman LA, Chow TW, Taber KH. The brainstem: anatomy, assessment, and clinical syndromes. J Neuropsychiatry Clin Neurosci. 2010;22(1):iv. doi: 10.1176/jnp.2010.22.1.iv.
- ↑ Annane D, Trabold F, Sharshar T, Jarrin I, Blanc AS, Raphael JC, et al. Inappropriate sympathetic activation at onset of septic shock: a spectral analysis approach. Am J Respir Crit Care Med août. 1999;160(2):458–465. doi: 10.1164/ajrccm.160.2.9810073.
- ↑ Sharshar T, Porcher R, Siami S, Rohaut B, Bailly-Salin J, Hopkinson NS, et al. Brainstem responses can predict death and delirium in sedated patients in intensive care unit. Crit Care Med août. 2011;39(8):1960–1967. doi: 10.1097/CCM.0b013e31821b843b.
- ↑ Sharshar T, Gray F, Lorin de la Grandmaison G, Hopkinson NS, Ross E, Dorandeu A, et al. Apoptosis of neurons in cardiovascular autonomic centres triggered by inducible nitric oxide synthase after death from septic shock. Lancet Lond Engl. 2003;362(9398):1799–1805. doi: 10.1016/S0140-6736(03)14899-4.
- ↑ Mazeraud A, Pascal Q, Verdonk F, Heming N, Chrétien F, Sharshar T. Neuroanatomy and physiology of brain dysfunction in sepsis. Clin Chest Med. 2016;37(2):333–345. doi: 10.1016/j.ccm.2016.01.013.
- ↑ Benghanem S, Mazeraud A, Azabou E, Chhor V, Shinotsuka CR, Claassen J, Rohaut B, Sharshar T. Brainstem dysfunction in critically ill patients. Crit Care. 2020 Jan 6;24(1):5. doi: 10.1186/s13054-019-2718-9.PMID: 31907011
- ↑ Chloé Gibeili, Arek Sulukdjian, Audrey Chanlon, Nathan Moreau. Unilateral glossodynia as a harbinger of an occult cerebellopontine angle tumour. BMJ Case Report.. 2022 Apr 12;15(4):e249408.doi: 10.1136/bcr-2022-249408.
- ↑ Irappa Madabhavi, Malay Sarkar, K S Sandeep, Mitul Modi. Isolated trigeminal neuralgia: An early weird presentation of carcinoma breast. J Cancer Res Ther. . 2022 Oct-Dec;18(6):1820-1822.doi: 10.4103/jcrt.JCRT_712_20.
- ↑ Advances in Head and Neck Cancer Pain. Ye Y, Jensen DD, Viet CT, Pan HL, Campana WM, Amit M, Boada MD.J Dent Res. 2022 Aug;101(9):1025-1033. doi: 10.1177/00220345221088527. Epub 2022 Apr 13.PMID: 35416080
- ↑ 10.0 10.1 Ramsey, I.S., M. Delling, and D.E. Clapham. 2006. An introduction to TRP channels. Annu Rev Physiol, 68: 619–647.
- ↑ 11.0 11.1 Julius, D. 2013. TRP channels and pain. Annu Rev Cell Dev Biol, 29: 355–584.
- ↑ Gutierrez, R., and S.A. Simon. 2011. Chemosensory processing in the taste-reward pathway. Flavour Fragr J, 26(4): 231–238.
- ↑ Carleton, A., R. Accolla, and S.A. Simon. 2010. Coding in the mammalian gustatory system. Trends Neurosci, 33(7): 326–334.
- ↑ Vincis, R. and A. Fontanini. 2016. A gustocentric perspective to understanding primary sensory cortices. Curr Opin Neurobiol, 40: 118–124
- ↑ Kaneko, Y., and A. Szallasi. 2014. Transient receptor potential (TRP) channels: A clinical perspective. Br J Pharmacol, 171(10): 2474–2507.
- ↑ Bourinet E, Altier C, Hildebrand M E, Trang T, Salter MW, Zamponi GW. Calcium permeable ion channels in pain signaling. Physiol Rev 2014; 94: 81–140.
- ↑ Jacobson A, Yang D, Vella M, Chiu IM (May 2021). "The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes". Mucosal Immunology. 14 (3): 555–565. doi:10.1038/s41385-020-00368-1. PMC 8075967. PMID 33542493.
- ↑ Khairatkar-Joshi N, Szallasi A (January 2009). "TRPV1 antagonists: the challenges for therapeutic targeting". Trends in Molecular Medicine. 15 (1): 14–22. doi:10.1016/j.molmed.2008.11.004. PMID 19097938.
- ↑ Jhaveri MD, Elmes SJ, Kendall DA, Chapman V (July 2005). "Inhibition of peripheral vanilloid TRPV1 receptors reduces noxious heat-evoked responses of dorsal horn neurons in naïve, carrageenan-inflamed and neuropathic rats". The European Journal of Neuroscience. 22 (2): 361–370. doi:10.1111/j.1460-9568.2005.04227.x. PMID 16045489. S2CID 24664751.
- ↑ Story GM, Crus-Orengo L (2008). "Feel the Burn". American Scientist. 95 (4): 326–333. doi:10.1511/2007.66.326. ISSN 0003-0996. Archived from the original on January 19, 2008.
- ↑ Gunthorpe MJ, Szallasi A (2008). "Peripheral TRPV1 receptors as targets for drug development: new molecules and mechanisms". Current Pharmaceutical Design. 14 (1): 32–41. doi:10.2174/138161208783330754. PMID 18220816.
- ↑ Boonen, Brett; Startek, Justyna B.; Talavera, Karel (2016-01-01). Chemical Activation of Sensory TRP Channels. Topics in Medicinal Chemistry. Springer Berlin Heidelberg. pp. 1–41. [1]doi:10.1007/7355_2015_98.
- ↑ 23.0 23.1 Yasunori Takayama, Daisuke Uta, Hidemasa Furue, and Makoto Tominaga. Pain-enhancing mechanism through interaction between TRPV1 and anoctamin 1 in sensory neurons. Proc Natl Acad Sci 2015; 21; 112(16): 5213-5218. doi: 10.1073/pnas.1421507112. Epub 2015 Apr 6.
- ↑ Z Yilmaz, T Renton, Y Yiangou, J Zakrzewska, I P Chessell, C Bountra, P Anand. Burning mouth syndrome as a trigeminal small fibre neuropathy: Increased heat and capsaicin receptor TRPV1 in nerve fibres correlates with pain score. J Clin Neurosci. 2007 Sep;14(9):864-71. doi: 10.1016/j.jocn.2006.09.002. Epub 2007 Jun 19.


![{\displaystyle \delta _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/cd35df3912a48e5b0b70d9cd5b2e1bee432c3272)










![{\displaystyle \gamma _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/2f85d0ed73fa3e7903f0321e48668467c1277f4e)
















![{\displaystyle \tau =[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/fbdc534cec0dcf1f070a551e40611eb83e8aca25)














