Difference between revisions of "The logic of the classical language"
| (16 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{main menu}} | {{main menu}} | ||
{{ArtBy| | {{ArtBy| | ||
| Line 21: | Line 6: | ||
| autore3 = Flavio Frisardi | | autore3 = Flavio Frisardi | ||
}} | }} | ||
==Introduction== | '''Abstract:''' This chapter explores the complexities of medical language, particularly within the context of diagnosis and treatment of Temporomandibular Disorders (TMD) and Orofacial Pain (OP). Medical language often leads to misunderstandings due to its hybrid nature, blending everyday language with specialized terms, which can be interpreted differently across medical disciplines. This is exemplified in the clinical case of Mary Poppins, who has suffered from OP for over a decade, with conflicting diagnoses from a dentist and a neurologist. The dentist diagnosed her with TMD based on clinical tests like axiography, electromyography (EMG), and radiographic imaging, while the neurologist attributed her pain to a neuromotor disorder (nOP). | ||
The chapter examines how classical logic language, used in traditional medical diagnostics, supports the dentist's diagnosis, focusing on the compatibility of evidence like condylar remodeling and masticatory muscle activity. However, the chapter also highlights the limitations of this approach, showing that new electrophysiological data could challenge the dentist’s assumptions and open the door to different interpretations of OP’s origins. | |||
In light of this, the chapter introduces the concept of "system logic language," which moves beyond cause-and-effect models to consider the masticatory system as a complex, dynamic entity. This perspective encourages a more nuanced understanding of patient conditions, recognizing that symptoms may not always align neatly with classical diagnostic frameworks. By analyzing Mary Poppins' case through both classical and system logic, the chapter calls for a reevaluation of medical language and diagnostic approaches, proposing a shift toward probabilistic and interdisciplinary methods for more accurate diagnoses. | |||
Ultimately, this chapter suggests that a deeper understanding of medical language and logic can improve clinical decision-making, reduce diagnostic errors, and foster a more comprehensive approach to patient care. | |||
==Introduction to the Logic of Medical Language== | |||
In the previous chapter, dedicated to the "[[Logic of medical language|Logic of Medical Language]]", we aimed to shift the focus from symptoms or clinical signs to an encrypted machine language. In this context, the arguments of Donald E. Stanley, Daniel G. Campos, and Pat Croskerry are particularly pertinent, especially when connected to the concept of time '''<math>t_n</math>''' as an information vector (anticipating the symptom) and to the consideration of the message as a machine language rather than a verbal language). | |||
<ref>{{Cite book | |||
| autore = Stanley DE | | autore = Stanley DE | ||
| autore2 = Campos DG | | autore2 = Campos DG | ||
| Line 55: | Line 49: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> | ||
We are | However, this does not lessen the importance of the clinical history, established on a pseudo-formal verbal language, which has now firmly entrenched itself in clinical practice and has proven its diagnostic effectiveness. Our aim in emphasizing a machine language and the system is merely to provide an additional opportunity to validate Medical-Diagnostic Science. We are fully aware that our "Linux Sapiens" remains puzzled by what has been anticipated and continues to ponder. | ||
{{q2|Could the logic of classical language help us solve the dilemma of poor Mary Poppins?|A bit of patience, please}} | |||
We cannot limit ourselves to providing a conventional answer, as science progresses not through baseless assertions but through questions and reflections that have passed the scrutiny of scientific validation. This compels us to explore and give voice to thoughts, perplexities, and doubts raised by certain key concepts discussed in various scientific articles. | |||
Among these critical topics is "'''Craniofacial Biology'''". | |||
==='''Craniofacial Biology'''=== | |||
We begin with an influential study by Townsend and Brook, | |||
<ref name=":0">{{Cite book | |||
| autore = Townsend GC | | autore = Townsend GC | ||
| autore2 = Brook AH | | autore2 = Brook AH | ||
| Line 80: | Line 78: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> in which the authors challenge the current research paradigm, both theoretical and applied, in "Craniofacial Biology", aiming to derive clinical considerations and implications. One aspect they address is the "Interdisciplinary Approach", through which Geoffrey Sperber and his son Steven recognized the potential for exponential growth in the field of "Craniofacial Biology" due to technological innovations such as gene sequencing, CT scans, MRI imaging, laser scanning, image analysis, ultrasound, and spectroscopy. | ||
<ref>{{Cite book | |||
| autore = Sperber GH | | autore = Sperber GH | ||
| autore2 = Sperber SM | | autore2 = Sperber SM | ||
| Line 97: | Line 96: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> | ||
Another topic of | Another topic of significant interest within 'Craniofacial Biology' is the recognition that biological systems are considered 'Complex Systems'. | ||
<ref>{{Cite book | |||
| autore = Brook AH | | autore = Brook AH | ||
| autore2 = Brook O'Donnell M | | autore2 = Brook O'Donnell M | ||
| Line 121: | Line 121: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> 'Epigenetics' also plays a fundamental role in craniofacial molecular biology. Researchers from Adelaide and Sydney have provided an in-depth critique in the field of epigenetics, with a particular focus on dental and craniofacial disciplines. | ||
<ref>{{Cite book | |||
| autore = Williams SD | | autore = Williams SD | ||
| autore2 = Hughes TE | | autore2 = Hughes TE | ||
| Line 141: | Line 142: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> Phenomics, in particular, | }}</ref> Phenomics, in particular, explored by these authors (see [[wikipedia:Phenomics|Phenomics]]), is a research area dedicated to measuring changes in teeth and associated orofacial structures resulting from interactions between genetic, epigenetic, and environmental factors during development. | ||
<ref>{{Cite book | |||
| autore = Yong R | | autore = Yong R | ||
| autore2 = Ranjitkar S | | autore2 = Ranjitkar S | ||
| Line 164: | Line 166: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> In this | }}</ref> | ||
In this context, it is crucial to mention the work of Irma Thesleff from Helsinki, Finland, who highlighted the existence of numerous transient signaling centers in the dental epithelium that play key roles in the tooth development program. | |||
<ref>{{Cite book | |||
| autore = Thesleff I | | autore = Thesleff I | ||
| titolo = Current understanding of the process of tooth formation: transfer from the laboratory to the clinic | | titolo = Current understanding of the process of tooth formation: transfer from the laboratory to the clinic | ||
| Line 180: | Line 184: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> | ||
Additionally, the works by Peterkova R., Hovorakova M., Peterka M., and Lesot H., offer a fascinating overview of the processes involved in dental development. | |||
<ref>{{Cite book | |||
| autore = Peterkova R | | autore = Peterkova R | ||
| autore2 = Hovorakova M | | autore2 = Hovorakova M | ||
| Line 243: | Line 250: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> For completeness, the studies by Han J., Menicanin D., Gronthos S., and Bartold P.M., which have explored a wide range of research on stem cells, tissue engineering, and periodontal regeneration, cannot be omitted. | ||
<ref>{{Cite book | |||
| autore = Han J | | autore = Han J | ||
| autore2 = Menicanin D | | autore2 = Menicanin D | ||
| Line 264: | Line 272: | ||
}}</ref> | }}</ref> | ||
This review necessarily included discussions on genetic, epigenetic, and environmental influences that, during morphogenesis, lead to variations in the number, size, and shape of teeth, | |||
<ref>{{Cite book | |||
<nowiki> </nowiki><nowiki>|</nowiki> autore = Brook AH | <nowiki> </nowiki><nowiki>|</nowiki> autore = Brook AH | ||
<nowiki> </nowiki><nowiki>|</nowiki> autore2 = Jernvall J | <nowiki> </nowiki><nowiki>|</nowiki> autore2 = Jernvall J | ||
| Line 299: | Line 308: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref> as well as on the effect of tongue pressure on growth and craniofacial functions. | ||
<ref>{{Cite book | |||
| autore = Kieser JA | | autore = Kieser JA | ||
| autore2 = Farland MG | | autore2 = Farland MG | ||
| Line 336: | Line 346: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref>Townsend and Brook | }}</ref> | ||
Furthermore, special mention is deserved for the exceptional work of Townsend and Brook, whose content aligns well with the reflections of another prominent author, HC Slavkin. Slavkin | |||
<ref>{{Cite book | |||
| autore = Slavkin HC | | autore = Slavkin HC | ||
| titolo = The Future of Research in Craniofacial Biology and What This Will Mean for Oral Health Professional Education and Clinical Practice | | titolo = The Future of Research in Craniofacial Biology and What This Will Mean for Oral Health Professional Education and Clinical Practice | ||
| Line 352: | Line 364: | ||
| LCCN = | | LCCN = | ||
| OCLC = | | OCLC = | ||
}}</ref> | }}</ref>asserts: | ||
{{ | The future holds countless opportunities to significantly improve the clinical outcomes of both congenital and acquired craniofacial malformations. Clinicians play a crucial role, as critical thinking combined with clinical experience greatly enhances diagnostic accuracy, and consequently, health outcomes.{{q2|I understand the progress of Science described by the authors but I do not understand the change in thought|Let me give you a practical example}} | ||
In the "[[Introduction]]", we raised some issues related to malocclusion. In this context, we examine the logic of the medical language used by the dentist when faced with the clinical case described in the "Introductory Chapter", including diagnostic and therapeutic conclusions. | |||
The patient has a unilateral posterior crossbite and an anterior open bite. | |||
<ref> | |||
The patient has a posterior | |||
{{cita libro | {{cita libro | ||
|autore=Littlewood SJ | |autore=Littlewood SJ | ||
| Line 377: | Line 387: | ||
|DOI=10.1111/adj.12475 | |DOI=10.1111/adj.12475 | ||
|OCLC= | |OCLC= | ||
}}</ref> The crossbite | }}</ref>The crossbite represents a deviation from normal occlusion | ||
<ref>{{cita libro | |||
|autore=Miamoto CB | |autore=Miamoto CB | ||
|autore2=Silva Marques L | |autore2=Silva Marques L | ||
| Line 393: | Line 404: | ||
|DOI= | |DOI= | ||
|OCLC= | |OCLC= | ||
}}</ref> | }}</ref> and is therefore treated concurrently with the open bite. | ||
<ref>{{cita libro | |||
|autore=Alachioti XS | |autore=Alachioti XS | ||
|autore2=Dimopoulou E | |autore2=Dimopoulou E | ||
| Line 423: | Line 435: | ||
|DOI=10.1179/bjo.5.1.21 | |DOI=10.1179/bjo.5.1.21 | ||
|OCLC= | |OCLC= | ||
}}</ref> This | }}</ref> This reasoning suggests that the model (masticatory system) is 'normalized to occlusion'; inversely interpreted, it implies that an occlusal discrepancy is a cause of malocclusion, that is, a disorder of the Masticatory System. Hence, an intervention to restore proper masticatory function is justified. (Figure 1a). | ||
---- | |||
This example is the classical logic language, as we will explain in detail, but now a doubt arises: | |||
<blockquote> | |||
At the time of formulating the orthodontic and orthognathic axioms, which led to the creation of protocols ratified by the International Scientific Community, were the information discussed in the introduction to this chapter already known? | |||
</blockquote> | |||
Certainly not, as the time '''<math>t_n</math>''' is a '''vector of information'''. However, despite this cognitive limitation, we proceed by adopting a classic language logic that raises relevant issues for citizen safety. | |||
{{q2|this statement seems a bit risky to me!|sure, but the logical sequence has already been anticipated}} | |||
If this case were analyzed through a mentality oriented towards a 'system language logic', which we will discuss in a dedicated chapter, the conclusions could be surprising. | |||
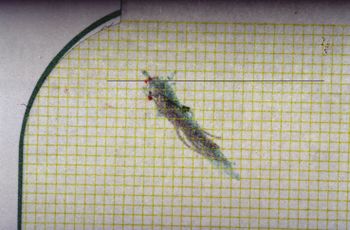
Analyzing the electrophysiological responses obtained from the patient with malocclusion, represented in figures 1b, 1c, and 1d (with explanations provided directly in the captions to facilitate the debate), it clearly emerges that these data lead us to considerations quite different from the simple 'Malocclusion'. Therefore, the orthodontic and orthognathic axioms based on a 'cause/effect' relationship show a significant conceptual gap. | |||
<gallery widths="350" heights="282" perrow="2" mode="slideshow"> | |||
File:Occlusal Centric view in open and cross bite patient.jpg| | File:Occlusal Centric view in open and cross bite patient.jpg|Figure 1a: Patient with malocclusion, open bite, and right posterior crossbite which in rehabilitative terms must be treated with orthodontic therapy and/or orthognathic surgery | ||
File:Bilateral Electric Transcranial Stimulation.jpg| | File:Bilateral Electric Transcranial Stimulation.jpg|Figure 1b: Motor evoked potential from transcranial electrical stimulation of the trigeminal roots. Note the structural symmetry calculated from the peak-to-peak amplitude on the left and right masseters (upper and lower traces respectively) | ||
File:Jaw Jerk .jpg| | File:Jaw Jerk .jpg|Figure 1c: Mandibular evoked reflex or mandibular jerk through percussion of the chin with a triggered neurological hammer. Note the functional symmetry calculated from the peak-to-peak amplitude on the left and right masseters (upper and lower traces respectively) | ||
File:Mechanic Silent Period.jpg| | File:Mechanic Silent Period.jpg|Figure 1d: Mechanically evoked silent period from percussion of the chin with a triggered neurological hammer. Note the functional symmetry calculated on the integral area of the right and left masseters (upper and lower traces respectively). | ||
</gallery> | </gallery> | ||
---- | ---- | ||
{{ | {{q2|So, how does the classic language logic connect to this context? |The contrast with the "system language logic" highlights the interpretive limits of traditional approaches to malocclusion. This suggests that orthodontic models of cause/effect might need a critical review in light of new electrophysiological evidence.}} | ||
== Mathematical Formalism== | |||
In this chapter, we will revisit the clinical case of Mary Poppins, who has been suffering from Orofacial Pain for over ten years, with a diagnosis of "Temporomandibular Disorder" (TMD) confirmed by her dentist, or, more specifically, Orofacial Pain associated with TMD. To understand the complexity in arriving at a precise diagnostic definition using Classic Language Logic, it is fundamental to introduce and analyze the concept at the basis of the philosophy of classical language. | |||
===Propositions=== | ===Propositions=== | ||
"The simplest propositions can be combined with each other to form new and more complex propositions through the use of logical operators and quantifier connectors. These tools of logic allow us to construct broader statements starting from basic concepts, thus facilitating the formulation of theorems and proofs in mathematics and other disciplines that require precision and rigor. | |||
The fundamental logical operators include: | |||
'' | *'''Conjunction''', denoted by the symbol <math>\land</math> (and): represents the logical operation "AND". A compound proposition formed by two propositions joined with "and" is true only if both propositions are true. | ||
*'''Disjunction''', denoted by the symbol <math>\lor</math> (or): represents the logical operation "OR". A compound proposition is true if at least one of the component propositions is true. | |||
*'''Negation''', denoted by the symbol <math>\urcorner</math> (not): reverses the truth value of a proposition. If a proposition is true, its negation is false, and vice versa. | |||
*'''Implication''', denoted by the symbol ⇒ (if... then): expresses a conditional relationship between two propositions. If the antecedent (first proposition) is true, then the consequent (second proposition) must be true for the implication to be true. | |||
*'''Logical consequence''', denoted by the symbol <math>\vdash</math> (it follows that): indicates that a proposition is a logical consequence of the previous ones within a given logical system. | |||
*'''Universal quantifier''', denoted by the symbol <math>\forall</math> (for all): expresses that the following proposition is true for all elements of a certain set. | |||
* '''Proof''', often indicated by reasonings that lead to the conclusion symbolized with <math>\mid</math> (thus): indicates the culmination of an argument or logical reasoning that leads to a conclusion. | |||
*'''Membership''', denoted by the symbol <math>\in</math> (belongs to) or <math>\not\in</math> (does not belong to): used to indicate whether an element belongs or does not belong to a set. | |||
Quantifier connectors, such as the universal quantifier (<math>\forall</math>) and the existential quantifier (<math>\exists</math>), allow for extending statements to sets of elements, offering a way to express propositions concerning 'all elements' of a certain set or 'at least one element' of such a set. | |||
=== | By combining these tools, it is possible to construct complex propositions that serve as the foundation for logical arguments and mathematical reasoning, eliminating the ambiguities typical of common language and providing a clear structure for analysis and proof." | ||
===Proof by Contradiction=== | |||
In classical logic, there exists a principle called "the law of excluded middle", which asserts that a proposition, which cannot be false, must be considered true, since there is no third possibility. | |||
Suppose we | Suppose we have to prove that the proposition p is true. The procedure consists of demonstrating that assuming <math>p</math> to be false leads to a logical contradiction. Consequently, the proposition <math>p</math> cannot be false and, therefore, according to the law of excluded middle, must be true. This method of proof is known as proof by contradiction.<ref>{{Cite book | ||
| author = Pereira LM | |||
| author2 = Pinto AM | |||
| title = Reductio ad Absurdum Argumentation in Normal Logic Programs | |||
| url = http://www-lia.deis.unibo.it/confs/ArgNMR/proceedings/ArgNMR-proceedings.pdf#page=100 | |||
| volume = Argumentation and Non-Monotonic Reasoning - An LPNMR Workshop | |||
| work = | |||
| year = 2007 | |||
| publisher = Arg NMR | |||
| city = Tempe, Arizona - Caparica, Portugal | |||
| ISBN = | |||
| PMID = | |||
| PMCID = | |||
| DOI = | |||
| oaf = <!-- any value --> | |||
| LCCN = | |||
| OCLC = | |||
}}</ref> | |||
===Predicates=== | |||
What has been briefly described so far represents the logic of propositions, which asserts something about specific mathematical objects. Examples of propositions include: "2 is greater than 1, therefore 1 is less than 2" or "a square does not have 5 sides, therefore it cannot be a pentagon". Often, however, mathematical statements are not limited to individual objects but refer to generic objects within a set, as in the expression "the elements ''<math>X</math>'' are taller than 2 meters", where ''<math>X</math>'' indicates a generic group (for example, all volleyball players). In these cases, we talk about predicates. | |||
Intuitively, a predicate is a sentence that concerns a set of elements (which, in our medical context, would be the patients) and makes a statement about them. | |||
{{q2|So, does Mary Poppins suffer from TMD or not?|let's see what classical language logic tells us}} | |||
In addition to the confirmations derived from the medical language logic discussed in the previous chapter, the dentist acquires further instrumental data that strengthen his diagnosis. These tests include the analysis of axiographic traces, obtained through the use of a custom-made functional paraocclusal fork. This tool allows for the visualization and quantification of the condylar paths during masticatory functions. As shown in Figure 4, the flattening of the condylar traces on the right side, both in the mediotrusive masticatory kinetics (indicated in green) and in the opening and protrusion cycles (in grey), confirms the anatomical and functional flattening of the right TMJ during the dynamics of mastication. | |||
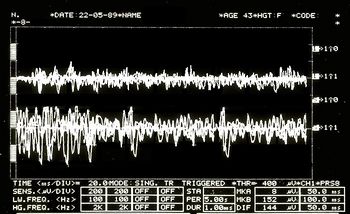
In addition to | In addition to axiography, surface electromyography on the masseter muscles is performed (see Figure 6), during which the patient is asked to exert maximum muscle force. This type of electromyographic analysis, called 'EMG Interferential Pattern', is characterized by the high-frequency content of the peaks showing phase interference. Indeed, Figure 6 highlights an asymmetry in the recruitment of motor units between the right masseter (upper trace) and the left masseter (lower trace). | ||
<ref>{{cite book | |||
| autore = Castroflorio T | | autore = Castroflorio T | ||
| autore2 = Talpone F | | autore2 = Talpone F | ||
| Line 563: | Line 583: | ||
==2nd Clinical Approach== | ==2nd Clinical Approach== | ||
(Hover over the images) | (Hover over the images) | ||
<gallery widths="350" heights="282" perrow="2" mode="slideshow"> | <gallery widths="350" heights="282" perrow="2" mode="slideshow"> | ||
File:Spasmo emimasticatorio.jpg| | File:Spasmo emimasticatorio.jpg|Figure 2: Patient reports "orofacial pain" on the right facial hemisphere. | ||
File:Spasmo emimasticatorio ATM.jpg| | File:Spasmo emimasticatorio ATM.jpg|Figure 3: Stratigraphy of the temporomandibular joint (TMJ) of the patient showing signs of condylar flattening and presence of osteophytes. | ||
File:Atm1 sclerodermia.jpg| | File:Atm1 sclerodermia.jpg|Figure 4: Computed tomography of the TMJ | ||
File:Spasmo emimasticatorio assiografia.jpg| | File:Spasmo emimasticatorio assiografia.jpg|Figure 5: Axiography of the patient showing a flattening of the masticatory pattern at the level of the right condyle. | ||
File:EMG2.jpg| | File:EMG2.jpg|Figure 6: Interfering EMG activity. Overlapping upper traces corresponding to the right masseter, below to the left masseter. | ||
</gallery> | </gallery></center> | ||
</center> | ---- | ||
=====Propositions in the Dental Context===== | |||
===== Dental | In an attempt to apply mathematical formalism to interpret the dentist's diagnostic conclusions using classical logic language, we define the following predicates: | ||
<math>x \equiv</math> Normal patients (where "normal" refers to patients commonly encountered in a specialist setting) | |||
<math>A(x) \equiv</math> Presence of bone remodeling with detected osteophyte from stratigraphic exams and condylar CT | |||
<math>B(x)\equiv</math> Temporomandibular Disorders (TMD) resulting in orofacial pain (OP) | |||
<math>\mathrm{a}\equiv</math> Specific patient: Mary Poppins | |||
We establish that for every normal patient <math>\mathrm{\mathcal{A}}(\text{x})</math>, if they test positive for the TMJ radiographic examination <math>\mathrm{\mathcal{A}}(\text{x})</math> [see Figures 2 and 3], then they are affected by TMD<math>\rightarrow\mathrm{\mathcal{B}}(\text{x})</math>. Consequently <math>\vdash</math> if Mary Poppins tests positive (and is considered a "normal patient") for the TMJ radiographic exam <math>A(a)</math>, it follows that she too is affected by TMD <math>\rightarrow \mathcal{B}(a)</math>. This can be formally expressed as: | |||
{| | |||
| | |||
|<math>{a \in x \mid \forall \text{x} ; A(\text{x}) \rightarrow {B}(\text{x}) \vdash A( a)\rightarrow B(a) } | |||
</math> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|<math>(1)</math> | |||
|} | |||
In | In addition to proving that a certain set of premises implies a particular conclusion, predicate logic is also used to prove the falsity of a statement or the logical compatibility/incompatibility of a certain piece of knowledge with a given piece of evidence. | ||
<math>\urcorner | To verify the truthfulness of this proposition, we resort to proof by contradiction. If the negation of the proposition generates a contradiction, we can conclude that the original hypothesis of the dentist is correct: | ||
{| | |||
| | |||
|<math>\urcorner{a \in x \mid \forall \text{x} ; A(\text{x}) \rightarrow {B}(\text{x}) \vdash A( a)\rightarrow B(a) }</math> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|<math>(2)</math> | |||
|} | |||
Statement (2) asserts that it is not true that patients who test positive for the TMJ CT are affected by TMD, implying that Mary Poppins (a "normal patient" with a positive outcome for the TMJ CT) is not affected by TMD. | |||
The dentist believes that this statement, based on the provided premises, constitutes a contradiction, thereby confirming the validity of the main statement. | |||
===Propositions in the Neurological Context=== | |||
Suppose the neurologist contests conclusion (1), arguing that Mary Poppins does not suffer from TMD or that, at least, TMD is not the primary cause of her Orofacial Pain. Instead, he hypothesizes that Mary suffers from neuromotor type Orofacial Pain (<sub>n</sub>OP), classifying her not as a 'normal patient' but as a 'specific patient' (atypical for the dental specialist). | |||
The neurologist's position can be formalized as follows: | |||
{| | |||
| | |||
|<math>{a \not\in x \mid \forall \text{x} ; A(\text{x}) \rightarrow {B}(\text{x}) \and A( a)\rightarrow \urcorner B(a) }</math> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|<math>(3)</math> | |||
|} | |||
This statement (3) claims that there might exist a patient with a positive outcome for the TMJ CT who does not suffer from TMD. To validate this hypothesis through proof by contradiction, consider its negation: | |||
{| | |||
| | |||
|<math>\urcorner{a \not\in x \mid \forall \text{x} ; A(\text{x}) \rightarrow {B}(\text{x}) \and A( a)\rightarrow \urcorner B(a) }</math> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|<math>(4)</math> | |||
|} | |||
Analyzing predicate logic, we find no sufficient reasons to believe that negation (4) leads to a contradiction, indicating that the neurologist, unlike the dentist, may not have sufficient logical grounds to confirm his conclusion without further evidence. | |||
{{q2|so the dentist triumphs!|don't take it for granted}} | |||
===Compatibility and Incompatibility of Statements === | |||
The complexity arises when the dentist presents a series of statements based on clinical reports, such as stratigraphy and computed tomography (CT) of the temporomandibular joint (TMJ), indicating an anatomical flattening of the joint, axiography of the condylar paths with a reduction of cinematic convexity, and an electromyographic (EMG) interference pattern showing asymmetry on the masseters. These evidences can be considered co-causes of damage to the temporomandibular joint and, consequently, responsible for "Orofacial Pain". | |||
Documents, reports, and clinical evidence can be used to make the neurologist's statement incompatible and support the dentist's diagnostic conclusion. To do this, we present some logical rules that describe compatibility or incompatibility according to classical language logic: | |||
<math>\ | #A set of sentences <math>\Im</math> and a number <math>n\geq1</math> of other sentences or statements <math>(\delta_1,\delta_2,.....\delta_n \ )</math> are logically compatible if, and only if, their union <math>\Im\cup{\delta_1,\delta_2.....\delta_n}</math> is coherent. | ||
#A set of sentences <math>\Im</math> and a number <math>n\geq1</math> of other sentences or statements <math>(\delta_1,\delta_2,.....\delta_n \ )</math> are logically incompatible if, and only if, their union <math>\Im\cup{\delta_1,\delta_2.....\delta_n}</math> is incoherent. | |||
Let's examine this concept with practical examples. | |||
The dentist presents the following statement: | |||
<math>\Im</math>: Following the personalized techniques suggested by Xin Liang et al. | |||
<ref>{{cite book | |||
<math>\Im</math>: Following the personalized techniques suggested by Xin Liang et al.<ref>{{cite book | |||
| autore = Liang X | | autore = Liang X | ||
| autore2 = Liu S | | autore2 = Liu S | ||
| Line 646: | Line 743: | ||
| DOI = 10.1016/j.oooo.2017.05.514 | | DOI = 10.1016/j.oooo.2017.05.514 | ||
| oaf = <!-- qualsiasi valore --> | | oaf = <!-- qualsiasi valore --> | ||
}}</ref> | }}</ref> that focuses on the quantitative microstructural analysis of the bone value fraction, trabecular number, trabecular thickness, and trabecular separation on each slice of a TMJ CT, it appears that Mary Poppins is affected by Temporomandibular Disorders (TMDs) and the consequence causes orofacial pain. | ||
However, to further confirm the diagnosis, the dentist presents a series of additional assertions that should pass the compatibility filter described above, thus establishing a coherent basis for the diagnosis of TMD in Mary Poppins. | |||
<math>\delta_1=</math> | '''<math>\delta_1=</math> Bone remodeling:''' The flattening of the axiographic traces shown in Figure 5 indicates the joint remodeling of Mary Poppins' right TMJ. This report can be related to a series of research and articles confirming how malocclusion can be associated with morphological changes of the temporomandibular joints, particularly if related to age. Indeed, the presence of chronic malocclusion can aggravate the scenario of bone remodeling. | ||
<ref>{{cite book | |||
| autore = Solberg WK | | autore = Solberg WK | ||
| autore2 = Bibb CA | | autore2 = Bibb CA | ||
| Line 667: | Line 765: | ||
| DOI = 10.1016/0002-9416(86)90055-2 | | DOI = 10.1016/0002-9416(86)90055-2 | ||
| oaf = <!-- qualsiasi valore --> | | oaf = <!-- qualsiasi valore --> | ||
}}</ref> | }}</ref> The provided scientific references support the compatibility of the assertion. | ||
'''<math>\delta_2=</math> Sensitivity and Specificity of the Axiographic Measurement:''' | |||
A study was conducted to evaluate the sensitivity and specificity of the data obtained from a sample of patients with temporomandibular joint disorders, using the ARCUSdigma axiographic system. | |||
<ref>[https://www.kavo.com/de-de/ KaVo Dental GmbH, Biberach / Ris]</ref> | |||
The results showed a sensitivity of 84.21% for the right TMJ and 92.86% for the left TMJ, with a specificity of 93.75% and 95.65%, respectively. | |||
<ref>{{cite book | |||
| autore = Kobs G | | autore = Kobs G | ||
| autore2 = Didziulyte A | | autore2 = Didziulyte A | ||
| Line 686: | Line 789: | ||
| DOI = | | DOI = | ||
| oaf = <!-- qualsiasi valore --> | | oaf = <!-- qualsiasi valore --> | ||
}}</ref> These | }}</ref> These scientifically validated data support the compatibility of the statement in the dental field, given the consistency of related studies. | ||
<ref>{{cite book | |||
| autore = Piancino MG | | autore = Piancino MG | ||
| autore2 = Roberi L | | autore2 = Roberi L | ||
| Line 706: | Line 810: | ||
}}</ref> | }}</ref> | ||
<math>\delta_3=</math> | '''<math>\delta_3=</math> Alteration in Condylar Paths:''' | ||
Urbano Santana-Mora and colleagues | |||
<ref>{{cite book | |||
| autore = López-Cedrún J | | autore = López-Cedrún J | ||
| autore2 = Santana-Mora U | | autore2 = Santana-Mora U | ||
| Line 726: | Line 833: | ||
| DOI = 10.1038/sdata.2017.168 | | DOI = 10.1038/sdata.2017.168 | ||
| oaf = YES<!-- qualsiasi valore --> | | oaf = YES<!-- qualsiasi valore --> | ||
}}</ref> | }}</ref> conducted a study on 24 adult patients suffering from severe chronic unilateral pain, diagnosed with Temporomandibular Disorders (TMD). The research focused on the analysis of various functional and dynamic factors, including masticatory function, the remodeling of the temporomandibular joint (TMJ) or condylar paths (CP), and lateral jaw movement or lateral guidance (LG). | ||
The CPs were evaluated using conventional axiography, while the LG was examined through kinesiographic tracing analysis. | |||
<ref>[https://www.myotronics.com/ Myotronics Inc., Kent, WA, US]</ref> | |||
It was found that seventeen patients, corresponding to 71% of the total sample, habitually preferred to chew on one side. The mean and standard deviation of the CP angles were 47.90 (± 9.24) degrees, while the mean of the LG angles was 42.95 (± 11.78) degrees. | |||
The | The study results contributed to the definition of a new paradigm for TMDs, suggesting that the side affected by the disorder might coincide with the habitual chewing side, especially when the lateral mandibular cinematic angle is flatter. This parameter further supports the dental assertion regarding the correlation between chewing habits and the development of TMDs. | ||
<math>\delta_4=</math> | '''<math>\delta_4=</math> EMG Interference Pattern:''' | ||
M.O. Mazzetto and collaborators | |||
<ref>{{cite book | |||
| autore = Oliveira Mazzetto M | | autore = Oliveira Mazzetto M | ||
| autore2 = Almeida Rodrigues C | | autore2 = Almeida Rodrigues C | ||
| Line 750: | Line 862: | ||
| DOI = 10.1590/0103-6440201302310 | | DOI = 10.1590/0103-6440201302310 | ||
| oaf = <!-- qualsiasi valore --> | | oaf = <!-- qualsiasi valore --> | ||
}}</ref> | }}</ref> demonstrated that there is a positive correlation between the electromyographic activity of the anterior temporal muscles and the masseter and the 'Cranio-Mandibular Index' (CMI), with a value of <math>P=0,01</math>. This suggests that the use of CMI to quantify the severity of Temporomandibular Disorders (TMD) and electromyography (EMG) to assess the function of the masticatory muscles can represent a significant diagnostic and therapeutic element. Such scientific references support the compatibility of the assertion. | ||
<math>\delta_n=</math> | <math>\delta_n=?</math> | ||
Given the evidence presented and the statements made, the dentist can legitimately claim that the set of sentences <math>\Im</math>, and a number <math>n\geq1</math> of other positive clinical assertions or data <math>(\delta_1,\delta_2,.....\delta_n \ )</math> are logically compatible. This is because their union, <math>\Im\cup{\delta_1,\delta_2.....\delta_n}</math>, turns out to be coherent. | |||
{{q2|Following classical language logic, the dentist is right!|It would seem so! But beware, only in their own dental context!}} | |||
This statement is so | This statement is so valid that the value of <math>P</math> could be extended indefinitely, even reaching an <math>\alpha=0</math>, which corresponds to infinite significance, as long as it remains within the specific context; however, it may not hold any significance in different contexts, such as the neurological one, for example. | ||
==Final Considerations== | |||
Within the scope of this observation, the application of Predicate Logic significantly contributes to strengthening the dentist's deductive process, concurrently solidifying the principle of excluded middle. This principle is emphasized by the coherence of the supplementary statements <math>(\delta_1,\delta_2,...,\delta_n)</math>, providing the dentist with a solid foundation for a coherent diagnosis and to affirm with certainty that 'Poor Mary Poppins is, without a shadow of a doubt, affected by TMD or not.' | |||
{{q2|And what if, as research advances, new phenomena emerge supporting the neurologist's theories rather than the dentist's?|}} | |||
---- | |||
In essence, considering the compatibility of the assertions <math>(\delta_1,\delta_2,.....\delta_n)</math>, coherently supporting that Orofacial Pain is caused by a Temporomandibular Disorder might become incompatible if another set of equally coherent assertions <math>(\gamma_1,\gamma_2,.....\gamma_n)</math> emerged. This scenario would pave the way for a new interpretation <math>\Im</math>: Mary Poppins could be suffering from Orofacial Pain due to a Neuromotor Disorder (<sub>n</sub>OP), not directly from Temporomandibular Disorders. Within the current medical language, such assertions remain purely theoretical, given that prevailing beliefs and opinions do not facilitate a rapid paradigm shift. | |||
Considering also the risk associated with such a change, the analysis of recent studies on the epidemiology of Temporomandibular Disorders | |||
<ref>{{cite book | autore = LeResche L | titolo = Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors | url = https://pubmed.ncbi.nlm.nih.gov/9260045/ | volume = | opera = Crit Rev Oral Biol Med | anno = 1997 | editore = | città = | ISBN = | PMID = 9260045 | PMCID = | DOI = 10.1177/10454411970080030401 | oaf = <!-- qualsiasi valore --> }}</ref> could prove useful. These studies indicate that, despite methodological and sampling differences, pain in the temporomandibular region is relatively common, affecting about 10% of the population. Therefore, it is reasonable to hypothesize that Mary Poppins could fall within this percentage, classifying her as a patient suffering from Orofacial Pain due to Temporomandibular Disorders (TMD). | |||
In conclusion, adopting a classical dichotomous approach in medical language, which tends to categorize conditions in black or white, fails to capture the numerous nuances present in clinical realities. Therefore, exploring a more flexible and suitable linguistic approach is necessary... | |||
{{q2|Could we then consider adopting a probabilistic type of linguistic logic?|perhaps}} | |||
{{Bib}} | {{Bib}} | ||
{{apm}} | {{apm}} | ||
<onlyinclude> | <onlyinclude> | ||
</onlyinclude | </onlyinclude> | ||
Latest revision as of 16:38, 19 October 2024
The logic of the classical language
Abstract: This chapter explores the complexities of medical language, particularly within the context of diagnosis and treatment of Temporomandibular Disorders (TMD) and Orofacial Pain (OP). Medical language often leads to misunderstandings due to its hybrid nature, blending everyday language with specialized terms, which can be interpreted differently across medical disciplines. This is exemplified in the clinical case of Mary Poppins, who has suffered from OP for over a decade, with conflicting diagnoses from a dentist and a neurologist. The dentist diagnosed her with TMD based on clinical tests like axiography, electromyography (EMG), and radiographic imaging, while the neurologist attributed her pain to a neuromotor disorder (nOP).
The chapter examines how classical logic language, used in traditional medical diagnostics, supports the dentist's diagnosis, focusing on the compatibility of evidence like condylar remodeling and masticatory muscle activity. However, the chapter also highlights the limitations of this approach, showing that new electrophysiological data could challenge the dentist’s assumptions and open the door to different interpretations of OP’s origins.
In light of this, the chapter introduces the concept of "system logic language," which moves beyond cause-and-effect models to consider the masticatory system as a complex, dynamic entity. This perspective encourages a more nuanced understanding of patient conditions, recognizing that symptoms may not always align neatly with classical diagnostic frameworks. By analyzing Mary Poppins' case through both classical and system logic, the chapter calls for a reevaluation of medical language and diagnostic approaches, proposing a shift toward probabilistic and interdisciplinary methods for more accurate diagnoses.
Ultimately, this chapter suggests that a deeper understanding of medical language and logic can improve clinical decision-making, reduce diagnostic errors, and foster a more comprehensive approach to patient care.
Introduction to the Logic of Medical Language
In the previous chapter, dedicated to the "Logic of Medical Language", we aimed to shift the focus from symptoms or clinical signs to an encrypted machine language. In this context, the arguments of Donald E. Stanley, Daniel G. Campos, and Pat Croskerry are particularly pertinent, especially when connected to the concept of time as an information vector (anticipating the symptom) and to the consideration of the message as a machine language rather than a verbal language). [1][2]
However, this does not lessen the importance of the clinical history, established on a pseudo-formal verbal language, which has now firmly entrenched itself in clinical practice and has proven its diagnostic effectiveness. Our aim in emphasizing a machine language and the system is merely to provide an additional opportunity to validate Medical-Diagnostic Science. We are fully aware that our "Linux Sapiens" remains puzzled by what has been anticipated and continues to ponder.
(A bit of patience, please)
We cannot limit ourselves to providing a conventional answer, as science progresses not through baseless assertions but through questions and reflections that have passed the scrutiny of scientific validation. This compels us to explore and give voice to thoughts, perplexities, and doubts raised by certain key concepts discussed in various scientific articles.
Among these critical topics is "Craniofacial Biology".
Craniofacial Biology
We begin with an influential study by Townsend and Brook, [3] in which the authors challenge the current research paradigm, both theoretical and applied, in "Craniofacial Biology", aiming to derive clinical considerations and implications. One aspect they address is the "Interdisciplinary Approach", through which Geoffrey Sperber and his son Steven recognized the potential for exponential growth in the field of "Craniofacial Biology" due to technological innovations such as gene sequencing, CT scans, MRI imaging, laser scanning, image analysis, ultrasound, and spectroscopy. [4]
Another topic of significant interest within 'Craniofacial Biology' is the recognition that biological systems are considered 'Complex Systems'. [5] 'Epigenetics' also plays a fundamental role in craniofacial molecular biology. Researchers from Adelaide and Sydney have provided an in-depth critique in the field of epigenetics, with a particular focus on dental and craniofacial disciplines. [6] Phenomics, in particular, explored by these authors (see Phenomics), is a research area dedicated to measuring changes in teeth and associated orofacial structures resulting from interactions between genetic, epigenetic, and environmental factors during development. [7] In this context, it is crucial to mention the work of Irma Thesleff from Helsinki, Finland, who highlighted the existence of numerous transient signaling centers in the dental epithelium that play key roles in the tooth development program. [8]
Additionally, the works by Peterkova R., Hovorakova M., Peterka M., and Lesot H., offer a fascinating overview of the processes involved in dental development. [9][10][11] For completeness, the studies by Han J., Menicanin D., Gronthos S., and Bartold P.M., which have explored a wide range of research on stem cells, tissue engineering, and periodontal regeneration, cannot be omitted. [12]
This review necessarily included discussions on genetic, epigenetic, and environmental influences that, during morphogenesis, lead to variations in the number, size, and shape of teeth, [13][14] as well as on the effect of tongue pressure on growth and craniofacial functions. [15][16] Furthermore, special mention is deserved for the exceptional work of Townsend and Brook, whose content aligns well with the reflections of another prominent author, HC Slavkin. Slavkin [17]asserts:
The future holds countless opportunities to significantly improve the clinical outcomes of both congenital and acquired craniofacial malformations. Clinicians play a crucial role, as critical thinking combined with clinical experience greatly enhances diagnostic accuracy, and consequently, health outcomes.
(Let me give you a practical example)
In the "Introduction", we raised some issues related to malocclusion. In this context, we examine the logic of the medical language used by the dentist when faced with the clinical case described in the "Introductory Chapter", including diagnostic and therapeutic conclusions.
The patient has a unilateral posterior crossbite and an anterior open bite. [18]The crossbite represents a deviation from normal occlusion [19] and is therefore treated concurrently with the open bite. [20][21] This reasoning suggests that the model (masticatory system) is 'normalized to occlusion'; inversely interpreted, it implies that an occlusal discrepancy is a cause of malocclusion, that is, a disorder of the Masticatory System. Hence, an intervention to restore proper masticatory function is justified. (Figure 1a).
This example is the classical logic language, as we will explain in detail, but now a doubt arises:
At the time of formulating the orthodontic and orthognathic axioms, which led to the creation of protocols ratified by the International Scientific Community, were the information discussed in the introduction to this chapter already known?
Certainly not, as the time is a vector of information. However, despite this cognitive limitation, we proceed by adopting a classic language logic that raises relevant issues for citizen safety.
(sure, but the logical sequence has already been anticipated)
If this case were analyzed through a mentality oriented towards a 'system language logic', which we will discuss in a dedicated chapter, the conclusions could be surprising.
Analyzing the electrophysiological responses obtained from the patient with malocclusion, represented in figures 1b, 1c, and 1d (with explanations provided directly in the captions to facilitate the debate), it clearly emerges that these data lead us to considerations quite different from the simple 'Malocclusion'. Therefore, the orthodontic and orthognathic axioms based on a 'cause/effect' relationship show a significant conceptual gap.
(The contrast with the "system language logic" highlights the interpretive limits of traditional approaches to malocclusion. This suggests that orthodontic models of cause/effect might need a critical review in light of new electrophysiological evidence.)
Mathematical Formalism
In this chapter, we will revisit the clinical case of Mary Poppins, who has been suffering from Orofacial Pain for over ten years, with a diagnosis of "Temporomandibular Disorder" (TMD) confirmed by her dentist, or, more specifically, Orofacial Pain associated with TMD. To understand the complexity in arriving at a precise diagnostic definition using Classic Language Logic, it is fundamental to introduce and analyze the concept at the basis of the philosophy of classical language.
Propositions
"The simplest propositions can be combined with each other to form new and more complex propositions through the use of logical operators and quantifier connectors. These tools of logic allow us to construct broader statements starting from basic concepts, thus facilitating the formulation of theorems and proofs in mathematics and other disciplines that require precision and rigor.
The fundamental logical operators include:
- Conjunction, denoted by the symbol (and): represents the logical operation "AND". A compound proposition formed by two propositions joined with "and" is true only if both propositions are true.
- Disjunction, denoted by the symbol (or): represents the logical operation "OR". A compound proposition is true if at least one of the component propositions is true.
- Negation, denoted by the symbol (not): reverses the truth value of a proposition. If a proposition is true, its negation is false, and vice versa.
- Implication, denoted by the symbol ⇒ (if... then): expresses a conditional relationship between two propositions. If the antecedent (first proposition) is true, then the consequent (second proposition) must be true for the implication to be true.
- Logical consequence, denoted by the symbol (it follows that): indicates that a proposition is a logical consequence of the previous ones within a given logical system.
- Universal quantifier, denoted by the symbol (for all): expresses that the following proposition is true for all elements of a certain set.
- Proof, often indicated by reasonings that lead to the conclusion symbolized with (thus): indicates the culmination of an argument or logical reasoning that leads to a conclusion.
- Membership, denoted by the symbol (belongs to) or (does not belong to): used to indicate whether an element belongs or does not belong to a set.
Quantifier connectors, such as the universal quantifier () and the existential quantifier (), allow for extending statements to sets of elements, offering a way to express propositions concerning 'all elements' of a certain set or 'at least one element' of such a set.
By combining these tools, it is possible to construct complex propositions that serve as the foundation for logical arguments and mathematical reasoning, eliminating the ambiguities typical of common language and providing a clear structure for analysis and proof."
Proof by Contradiction
In classical logic, there exists a principle called "the law of excluded middle", which asserts that a proposition, which cannot be false, must be considered true, since there is no third possibility.
Suppose we have to prove that the proposition p is true. The procedure consists of demonstrating that assuming to be false leads to a logical contradiction. Consequently, the proposition cannot be false and, therefore, according to the law of excluded middle, must be true. This method of proof is known as proof by contradiction.[22]
Predicates
What has been briefly described so far represents the logic of propositions, which asserts something about specific mathematical objects. Examples of propositions include: "2 is greater than 1, therefore 1 is less than 2" or "a square does not have 5 sides, therefore it cannot be a pentagon". Often, however, mathematical statements are not limited to individual objects but refer to generic objects within a set, as in the expression "the elements are taller than 2 meters", where indicates a generic group (for example, all volleyball players). In these cases, we talk about predicates.
Intuitively, a predicate is a sentence that concerns a set of elements (which, in our medical context, would be the patients) and makes a statement about them.
(let's see what classical language logic tells us)
In addition to the confirmations derived from the medical language logic discussed in the previous chapter, the dentist acquires further instrumental data that strengthen his diagnosis. These tests include the analysis of axiographic traces, obtained through the use of a custom-made functional paraocclusal fork. This tool allows for the visualization and quantification of the condylar paths during masticatory functions. As shown in Figure 4, the flattening of the condylar traces on the right side, both in the mediotrusive masticatory kinetics (indicated in green) and in the opening and protrusion cycles (in grey), confirms the anatomical and functional flattening of the right TMJ during the dynamics of mastication.
In addition to axiography, surface electromyography on the masseter muscles is performed (see Figure 6), during which the patient is asked to exert maximum muscle force. This type of electromyographic analysis, called 'EMG Interferential Pattern', is characterized by the high-frequency content of the peaks showing phase interference. Indeed, Figure 6 highlights an asymmetry in the recruitment of motor units between the right masseter (upper trace) and the left masseter (lower trace).
2nd Clinical Approach
(Hover over the images)
Propositions in the Dental Context
In an attempt to apply mathematical formalism to interpret the dentist's diagnostic conclusions using classical logic language, we define the following predicates:
Normal patients (where "normal" refers to patients commonly encountered in a specialist setting) Presence of bone remodeling with detected osteophyte from stratigraphic exams and condylar CT Temporomandibular Disorders (TMD) resulting in orofacial pain (OP) Specific patient: Mary Poppins We establish that for every normal patient , if they test positive for the TMJ radiographic examination [see Figures 2 and 3], then they are affected by TMD. Consequently if Mary Poppins tests positive (and is considered a "normal patient") for the TMJ radiographic exam , it follows that she too is affected by TMD . This can be formally expressed as:
In addition to proving that a certain set of premises implies a particular conclusion, predicate logic is also used to prove the falsity of a statement or the logical compatibility/incompatibility of a certain piece of knowledge with a given piece of evidence.
To verify the truthfulness of this proposition, we resort to proof by contradiction. If the negation of the proposition generates a contradiction, we can conclude that the original hypothesis of the dentist is correct:
Statement (2) asserts that it is not true that patients who test positive for the TMJ CT are affected by TMD, implying that Mary Poppins (a "normal patient" with a positive outcome for the TMJ CT) is not affected by TMD.
The dentist believes that this statement, based on the provided premises, constitutes a contradiction, thereby confirming the validity of the main statement.
Propositions in the Neurological Context
Suppose the neurologist contests conclusion (1), arguing that Mary Poppins does not suffer from TMD or that, at least, TMD is not the primary cause of her Orofacial Pain. Instead, he hypothesizes that Mary suffers from neuromotor type Orofacial Pain (nOP), classifying her not as a 'normal patient' but as a 'specific patient' (atypical for the dental specialist).
The neurologist's position can be formalized as follows:
This statement (3) claims that there might exist a patient with a positive outcome for the TMJ CT who does not suffer from TMD. To validate this hypothesis through proof by contradiction, consider its negation:
Analyzing predicate logic, we find no sufficient reasons to believe that negation (4) leads to a contradiction, indicating that the neurologist, unlike the dentist, may not have sufficient logical grounds to confirm his conclusion without further evidence.
(don't take it for granted)
Compatibility and Incompatibility of Statements
The complexity arises when the dentist presents a series of statements based on clinical reports, such as stratigraphy and computed tomography (CT) of the temporomandibular joint (TMJ), indicating an anatomical flattening of the joint, axiography of the condylar paths with a reduction of cinematic convexity, and an electromyographic (EMG) interference pattern showing asymmetry on the masseters. These evidences can be considered co-causes of damage to the temporomandibular joint and, consequently, responsible for "Orofacial Pain".
Documents, reports, and clinical evidence can be used to make the neurologist's statement incompatible and support the dentist's diagnostic conclusion. To do this, we present some logical rules that describe compatibility or incompatibility according to classical language logic:
- A set of sentences and a number of other sentences or statements are logically compatible if, and only if, their union is coherent.
- A set of sentences and a number of other sentences or statements are logically incompatible if, and only if, their union is incoherent.
Let's examine this concept with practical examples.
The dentist presents the following statement:
: Following the personalized techniques suggested by Xin Liang et al. [27] that focuses on the quantitative microstructural analysis of the bone value fraction, trabecular number, trabecular thickness, and trabecular separation on each slice of a TMJ CT, it appears that Mary Poppins is affected by Temporomandibular Disorders (TMDs) and the consequence causes orofacial pain.
However, to further confirm the diagnosis, the dentist presents a series of additional assertions that should pass the compatibility filter described above, thus establishing a coherent basis for the diagnosis of TMD in Mary Poppins.
Bone remodeling: The flattening of the axiographic traces shown in Figure 5 indicates the joint remodeling of Mary Poppins' right TMJ. This report can be related to a series of research and articles confirming how malocclusion can be associated with morphological changes of the temporomandibular joints, particularly if related to age. Indeed, the presence of chronic malocclusion can aggravate the scenario of bone remodeling. [28] The provided scientific references support the compatibility of the assertion.
Sensitivity and Specificity of the Axiographic Measurement:
A study was conducted to evaluate the sensitivity and specificity of the data obtained from a sample of patients with temporomandibular joint disorders, using the ARCUSdigma axiographic system. [29] The results showed a sensitivity of 84.21% for the right TMJ and 92.86% for the left TMJ, with a specificity of 93.75% and 95.65%, respectively. [30] These scientifically validated data support the compatibility of the statement in the dental field, given the consistency of related studies. [31]
Alteration in Condylar Paths:
Urbano Santana-Mora and colleagues [32] conducted a study on 24 adult patients suffering from severe chronic unilateral pain, diagnosed with Temporomandibular Disorders (TMD). The research focused on the analysis of various functional and dynamic factors, including masticatory function, the remodeling of the temporomandibular joint (TMJ) or condylar paths (CP), and lateral jaw movement or lateral guidance (LG).
The CPs were evaluated using conventional axiography, while the LG was examined through kinesiographic tracing analysis. [33] It was found that seventeen patients, corresponding to 71% of the total sample, habitually preferred to chew on one side. The mean and standard deviation of the CP angles were 47.90 (± 9.24) degrees, while the mean of the LG angles was 42.95 (± 11.78) degrees.
The study results contributed to the definition of a new paradigm for TMDs, suggesting that the side affected by the disorder might coincide with the habitual chewing side, especially when the lateral mandibular cinematic angle is flatter. This parameter further supports the dental assertion regarding the correlation between chewing habits and the development of TMDs.
EMG Interference Pattern:
M.O. Mazzetto and collaborators [34] demonstrated that there is a positive correlation between the electromyographic activity of the anterior temporal muscles and the masseter and the 'Cranio-Mandibular Index' (CMI), with a value of . This suggests that the use of CMI to quantify the severity of Temporomandibular Disorders (TMD) and electromyography (EMG) to assess the function of the masticatory muscles can represent a significant diagnostic and therapeutic element. Such scientific references support the compatibility of the assertion.
Given the evidence presented and the statements made, the dentist can legitimately claim that the set of sentences , and a number of other positive clinical assertions or data are logically compatible. This is because their union, , turns out to be coherent.
(It would seem so! But beware, only in their own dental context!)
This statement is so valid that the value of could be extended indefinitely, even reaching an , which corresponds to infinite significance, as long as it remains within the specific context; however, it may not hold any significance in different contexts, such as the neurological one, for example.
Final Considerations
Within the scope of this observation, the application of Predicate Logic significantly contributes to strengthening the dentist's deductive process, concurrently solidifying the principle of excluded middle. This principle is emphasized by the coherence of the supplementary statements , providing the dentist with a solid foundation for a coherent diagnosis and to affirm with certainty that 'Poor Mary Poppins is, without a shadow of a doubt, affected by TMD or not.'
In essence, considering the compatibility of the assertions , coherently supporting that Orofacial Pain is caused by a Temporomandibular Disorder might become incompatible if another set of equally coherent assertions emerged. This scenario would pave the way for a new interpretation : Mary Poppins could be suffering from Orofacial Pain due to a Neuromotor Disorder (nOP), not directly from Temporomandibular Disorders. Within the current medical language, such assertions remain purely theoretical, given that prevailing beliefs and opinions do not facilitate a rapid paradigm shift.
Considering also the risk associated with such a change, the analysis of recent studies on the epidemiology of Temporomandibular Disorders [35] could prove useful. These studies indicate that, despite methodological and sampling differences, pain in the temporomandibular region is relatively common, affecting about 10% of the population. Therefore, it is reasonable to hypothesize that Mary Poppins could fall within this percentage, classifying her as a patient suffering from Orofacial Pain due to Temporomandibular Disorders (TMD).
In conclusion, adopting a classical dichotomous approach in medical language, which tends to categorize conditions in black or white, fails to capture the numerous nuances present in clinical realities. Therefore, exploring a more flexible and suitable linguistic approach is necessary...
(perhaps)
- ↑ Stanley DE, Campos DG, «The logic of medical diagnosis», in Perspect Biol Med, 2013».
PMID:23974509
DOI:10.1353/pbm.2013.0019 - ↑ Croskerry P, «Adaptive expertise in medical decision making», in Med Teach, 2018».
PMID:30033794
DOI:10.1080/0142159X.2018.1484898 - ↑ Townsend GC, Brook AH, «The face, the future, and dental practice: how research in craniofacial biology will influence patient care», in Aust Dent J, Australian Dental Association, 2014».
PMID:24646132
DOI:10.1111/adj.12157 - ↑ Sperber GH, Sperber SM, «The genesis of craniofacial biology as a health science discipline», in Aust Dent J, Australian Dental Association, 2014».
PMID:24495071
DOI:10.1111/adj.12131 - ↑ Brook AH, Brook O'Donnell M, Hone A, Hart E, Hughes TE, Smith RN, Townsend GC, «General and craniofacial development are complex adaptive processes influenced by diversity», in Aust Dent J, Australian Dental Association, 2014».
PMID:24617813
DOI:10.1111/adj.12158 - ↑ Williams SD, Hughes TE, Adler CJ, Brook AH, Townsend GC, «Epigenetics: a new frontier in dentistry», in Aust Dent J, Australian Dental Association, 2014».
PMID:24611746
DOI:10.1111/adj.12155 - ↑ Yong R, Ranjitkar S, Townsend GC, Brook AH, Smith RN, Evans AR, Hughes TE, Lekkas D, «Dental phenomics: advancing genotype to phenotype correlations in craniofacial research», in Aust Dent J, Australian Dental Association, 2014».
PMID:24611797
DOI:10.1111/adj.12156 - ↑ Thesleff I, «Current understanding of the process of tooth formation: transfer from the laboratory to the clinic», in Aust Dent J, 2013».
DOI:10.1111/adj.12102 - ↑ Peterkova R, Hovorakova M, Peterka M, Lesot H, «Three‐dimensional analysis of the early development of the dentition», in Aust Dent J, Wiley Publishing Asia Pty Ltd on behalf of Australian Dental Association, 2014».
DOI:10.1111/adj.12130 - ↑ Lesot H, Hovorakova M, Peterka M, Peterkova R, «Three‐dimensional analysis of molar development in the mouse from the cap to bell stage», in Aust Dent J, 2014».
DOI:10.1111/adj.12132 - ↑ Hughes TE, Townsend GC, Pinkerton SK, Bockmann MR, Seow WK, Brook AH, Richards LC, Mihailidis S, Ranjitkar S, Lekkas D, «The teeth and faces of twins: providing insights into dentofacial development and oral health for practising oral health professionals», in Aust Dent J, 2013».
DOI:10.1111/adj.12101 - ↑ Han J, Menicanin D, Gronthos S, Bartold PM, «Stem cells, tissue engineering and periodontal regeneration», in Aust Dent J, 2013».
DOI:10.1111/adj.12100 - ↑ {{Cite book | autore = Brook AH | autore2 = Jernvall J | autore3 = Smith RN | autore4 = Hughes TE | autore5 = Townsend GC | titolo = The Dentition: The Outcomes of Morphogenesis Leading to Variations of Tooth Number, Size and Shape | url = https://onlinelibrary.wiley.com/doi/epdf/10.1111/adj.12160 | volume = | opera = Aust Dent J | anno = 2014 | editore = | città = | ISBN = | PMID = | PMCID = | DOI = 10.1111/adj.12160 | oaf = | LCCN = | OCLC =
- ↑ Seow WK, «Developmental defects of enamel and dentine: challenges for basic science research and clinical management», in Aust Dent J, 2014».
PMID:24164394
DOI:10.1111/adj.12104 - ↑ Kieser JA, Farland MG, Jack H, Farella M, Wang Y, Rohrle O, «The role of oral soft tissues in swallowing function: what can tongue pressure tell us?», in Aust Dent J, 2013».
DOI:10.1111/adj.12103 - ↑ Slavkin HC, «Research on Craniofacial Genetics and Developmental Biology: Implications for the Future of Academic Dentistry», in J Dent Educ, 1983».
PMID:6573384 - ↑ Slavkin HC, «The Future of Research in Craniofacial Biology and What This Will Mean for Oral Health Professional Education and Clinical Practice», in Aust Dent J, 2014».
PMID:24433547
DOI:10.1111/adj.12105 - ↑
Littlewood SJ, Kandasamy S, Huang G, «Retention and relapse in clinical practice», in Aust Dent J, 2017».
DOI:10.1111/adj.12475 - ↑ Miamoto CB, Silva Marques L, Abreu LG, Paiva SM, «Impact of two early treatment protocols for anterior dental crossbite on children’s quality of life», in Dental Press J Orthod, 2018».
- ↑ Alachioti XS, Dimopoulou E, Vlasakidou A, Athanasiou AE, «Amelogenesis imperfecta and anterior open bite: Etiological, classification, clinical and management interrelationships», in J Orthod Sci, 2014».
DOI:10.4103/2278-0203.127547 - ↑ Mizrahi E, «A review of anterior open bite», in Br J Orthod, 1978».
PMID:284793
DOI:10.1179/bjo.5.1.21 - ↑ «[1]» – in «Argumentation and Non-Monotonic Reasoning - An LPNMR Workshop».
- ↑ Castroflorio T, Talpone F, Deregibus A, Piancino MG, Bracco P, «Effects of a Functional Appliance on Masticatory Muscles of Young Adults Suffering From Muscle-Related Temporomandibular Disorder», in J Oral Rehabil, 2004».
PMID:15189308
DOI:10.1111/j.1365-2842.2004.01274.x - ↑ Maeda N, Kodama N, Manda Y, Kawakami S, Oki K, Minagi S, «Characteristics of Grouped Discharge Waveforms Observed in Long-term Masseter Muscle Electromyographic Recording: A Preliminary Study», in Acta Med Okayama, Okayama University Medical School, 2019, Okayama, Japan».
PMID:31439959
DOI:10.18926/AMO/56938 - ↑ Rudy TE, «Psychophysiological Assessment in Chronic Orofacial Pain», in Anesth Prog, American Dental Society of Anesthesiology, 1990».
ISSN: 0003-3006/90
PMID:2085203 - PMCID:PMC2190318 - ↑ Woźniak K, Piątkowska D, Lipski M, Mehr K, «Surface electromyography in orthodontics - a literature review», in Med Sci Monit, 2013».
e-ISSN: 1643-3750
PMID:23722255 - PMCID:PMC3673808
DOI:10.12659/MSM.883927 - ↑ Liang X, Liu S, Qu X, Wang Z, Zheng J, Xie X, Ma G, Zhang Z, Ma X, «Evaluation of Trabecular Structure Changes in Osteoarthritis of the Temporomandibular Joint With Cone Beam Computed Tomography Imaging», in Oral Surg Oral Med Oral Pathol Oral Radiol, 2017».
PMID:28732700
DOI:10.1016/j.oooo.2017.05.514 - ↑ Solberg WK, Bibb CA, Nordström BB, Hansson TL, «Malocclusion Associated With Temporomandibular Joint Changes in Young Adults at Autopsy», in Am J Orthod, 1986».
PMID:3457531
DOI:10.1016/0002-9416(86)90055-2 - ↑ KaVo Dental GmbH, Biberach / Ris
- ↑ Kobs G, Didziulyte A, Kirlys R, Stacevicius M, «Reliability of ARCUSdigma (KaVo) in Diagnosing Temporomandibular Joint Pathology», in Stomatologija, 2007».
PMID:17637527 - ↑ Piancino MG, Roberi L, Frongia G, Reverdito M, Slavicek R, Bracco P, «Computerized axiography in TMD patients before and after therapy with 'function generating bites'», in J Oral Rehabil, 2008».
PMID:18197841
DOI:10.1111/j.1365-2842.2007.01815.x - ↑ López-Cedrún J, Santana-Mora U, Pombo M, Pérez Del Palomar A, Alonso De la Peña V, Mora MJ, Santana U, «Jaw Biodynamic Data for 24 Patients With Chronic Unilateral Temporomandibular Disorder», in Sci Data, 2017».
PMID:29112190 - PMCID:PMC5674825
DOI:10.1038/sdata.2017.168
This is an Open Access resource! - ↑ Myotronics Inc., Kent, WA, US
- ↑ Oliveira Mazzetto M, Almeida Rodrigues C, Valencise Magri L, Oliveira Melchior M, Paiva G, «Severity of TMD Related to Age, Sex and Electromyographic Analysis», in Braz Dent J, 2014».
DOI:10.1590/0103-6440201302310 - ↑ LeResche L, «Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors», in Crit Rev Oral Biol Med, 1997».
PMID:9260045
DOI:10.1177/10454411970080030401
particularly focusing on the field of the neurophysiology of the masticatory system