|
|
| (6 intermediate revisions by the same user not shown) |
| Line 1: |
Line 1: |
| == Introduzione== | | {{main menu}}{{ArtBy| |
| | | autore = Gianni Frisardi |
| | | autore2 = |
| | | autore3 = |
| | }} |
|
| |
|
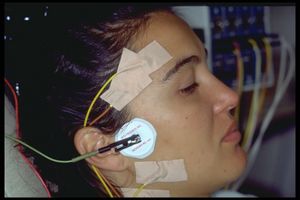
| | [[File:Myomonitor.jpg|left|frameless]] |
| | In this chapter, we consider another highly debated topic: Transcutaneous Electrical Nerve Stimulation (TENS), on which there is still no unanimous opinion within the International Scientific Community. This premise is confirmed by the fact that, although the Research Diagnostic Criteria (RDC) have categorically invalidated the clinical procedure in diagnosing patients with Temporomandibular Disorders, the procedure is still considered valid. It continues to be discussed, articles are published, and it is still practiced. This inconsistency is demonstrated by scientific papers in the literature with intermediate and ambiguous conclusions, which generate only questions without providing valid answers. |
|
| |
|
| In questo capitolo prendiamo in considerazione un altro argomento molto dibattuto, quello della Stimolazione Elettrica Transcutanea (TENS), su cui ancora non c'è una opinione univoca nella Comunità Scientifica Internazionale. Questa premessa viene confermata dal fatto che nonostante lo Research Diagnostic Criteria (RDC) abbia categoricamente invalidato la procedura clinica nella diagnostica dei pazienti affetti da Disordini Temporomandibolari, ancora viene considerata valida, visto che se ne parla, si pubblicano articoli ma sostanzialmente si pratica ancora come procedura clinica. Questo controsenso può essere verificato da lavori scientifici in letteratura con conclusioni intermedie ed ambigue che generano di conseguenza solo domande e non conclusioni valide.
| | The RDC has clinically deemed the TENS procedure invalid based on the freeway space and myocentric trajectory, both as diagnostic elements for Temporomandibular Disorders (TMD) and as part of masticatory prosthetic rehabilitation treatment. As can be seen from the specific section of Table 1 presented in the chapter [[Research Diagnostic Criteria (RDC)]], it is clear that both freeway space and TENS trajectory were excluded due to a low predictive value (PPV: 0.17). While this might be true, it is essential to delve into the technical and methodological details to understand the rationale behind this decision. For this reason, we will briefly but thoroughly describe the TENS method to better understand its weaknesses and strengths. |
|
| |
|
| Sostanzialmente lo RDC ha considerato non valido clinicamente la procedura con TENS sulla base del free way space e della traiettoria della miocentrica che sia come elemento di diagnosi nei Disordini Temporomandibolare che per il trattamento delle riabilitazioni protesiche masticatorie. Come si può notare dallo specifica sezione della tabella 1 presentata nel capitolo Stimolazione Elettrica Transcutanea si evince che sia il fre way space che la traiettoria con TENS siano state escluse per un valore predittivo troppo basso. Tutto questo potrebbe essere anche vero ma è essenziale scendere in profondità tecniche e metodologiche per capire quanto c'è di vero e di giustificabile in certe prese di posizioni oppure se è solo un modo non corretto di impiegare il metodo. Per questo motivo è auspicabile in primis descrivere brevemente ma dettagliatamente il metodo TENS e poi capire quali sono i punti deboli e forza della metodica.
| | '''TENS and Temporomandibular Disorders:''' The temporomandibular joint (TMJ) is a hinge joint with biarticular properties, enabling the complex movements required for chewing. Temporomandibular disorder (TMD) occurs when the TMJ and associated anatomical structures are affected. Approximately 25% of individuals worldwide show signs or symptoms of TMD. TMD occurs 1.5 to 2.5 times more frequently in women than in men. |
| {| class="wikitable"
| |
| | colspan="5" |'''Table 1:''' DTM diagnostic methodologies analyzed and eliminated from the DRC because they are not scientifically validated
| |
| |-
| |
| |'''Diagnostic Tests'''
| |
| |'''Cutoff'''
| |
| |'''Sensitivity'''
| |
| |'''Specificity'''
| |
| |'''VPP'''
| |
| |-
| |
| | colspan="5" |'''Electrical stimulation methods'''
| |
| |-
| |
| |Free rest space before stimulation''( Cooper e Rabuzzi 1984)''<ref name=":1" />
| |
| |0.75-2.0 mm
| |
| |0.42
| |
| |0.62
| |
| |0.17
| |
| |-
| |
| |Free space to rest after electric-stimulation ''( Cooper e Rabuzzi 1984;''<ref name=":1" />)
| |
| |0.75-2.0 mm
| |
| |0.76
| |
| |0.19
| |
| |0.11
| |
| |-
| |
| |Closure trajectory before after electrical stimulation''( Cooper e Rabuzzi 1984)''<ref name=":1" />
| |
| |Non definita
| |
| |0.75
| |
| |0.27
| |
| |0.12
| |
| |-
| |
| | colspan="5" |<small>Cutoff: Parameters and limits of significance that should divide sick from healthy, for each test reported</small><small>Sensitivity: Ability of the specified test to identify the truly sick in a sample of healthy and sick subjects</small>
| |
|
| |
|
| <small>Specificity: Ability of the specified test to identify the healthy in a sample of healthy and sick subjects</small>
| | Various therapeutic approaches are being studied for managing TMD, aiming to relieve pain and improve jaw function. Although surgical and non-surgical methods are available for treating TMD, conservative treatment is the initial and primary option. Pharmacological therapies include the use of nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, and muscle relaxants. Another treatment component consists of occlusal and physical therapy techniques, such as low-level laser therapy (LLLT) and Transcutaneous Electrical Nerve Stimulation of the trigeminal nerve (TENS). |
|
| |
|
| <small>Positive Predictive Value (PPV): Ratio of the ability of the specified test to identify truly sick (positive) patients on the total sick population in a sample of healthy and sick subjects.</small>
| | TENS has gained recognition as a non-invasive and drug-free technique for pain management in TMD. It involves applying low-frequency electrical currents to the skin through surface electrodes. These currents stimulate sensory nerves and modulate pain signals transmitted to the central nervous system (CNS), altering pain perception. TENS is used in TMD patients to target muscles and nerves surrounding the TMJ, promoting muscle relaxation, reducing muscle spasms, and relieving discomfort. |
| |}
| | . |
|
| |
|
| === TENS e Disordini Temporomandibolari ===
| | '''Conclusion:''' Despite the controversy surrounding TENS in the treatment of TMD, studies show varying degrees of efficacy in pain reduction and muscle relaxation. However, its role compared to other treatment modalities remains unclear and requires further research to establish its definitive clinical utility.{{Login or request Member account}} |
| L'articolazione temporo-mandibolare (TMJ) è un'articolazione a cerniera con proprietà biartrodiali, che consente i movimenti complessi richiesti per la masticazione<ref>Okoje VN, Aladelusi TO, Abimbola TA. Managing temporomandibular joint dislocation in ibadan: a review of 11 cases. Ann Ib Postgrad Med 2017;15:96-10</ref>. Il disturbo temporo-mandibolare (TMD) si verifica quando la TMJ e le strutture anatomiche associate sono colpite<ref>Maini K, Dua A. Temporomandibular Syndrome. Treasure Island, FL: StatPearls Publishing; 2024</ref><ref>Murphy MK, MacBarb RF, Wong ME, Athanasiou KA. Temporomandibular disorders: a review of etiology, clinical management, and tissue engineering strategies. Int J Oral Maxillofac Implants 2013;28:e393-414. doi: 10.11607/jomi.te20</ref>. Circa il 25% degli individui a livello globale mostra segni o sintomi di TMD<ref>Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs 2001;169:187-92. doi: 10.1159/000047881</ref>. Inoltre, i TMD si verificano 1,5-2,5 volte più frequentemente nelle donne rispetto agli uomini<ref>Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs 2001;169:187-92. doi: 10.1159/000047881</ref>. Si tratta di un disturbo prevalente, caratterizzato da dolore, disfunzione e disagio nella TMJ e nelle strutture circostanti, che influisce su una parte significativa della popolazione, limitando le attività quotidiane, riducendo la qualità della vita e aumentando i costi sanitari<ref>Kapos FP, Exposto FG, Oyarzo JF, Durham J. Temporomandibular disorders: a review of current concepts in aetiology, diagnosis and management. Oral Surg 2020;13:321-34. doi: 10.1111/ors.12473</ref><ref>Alrizqi AH, Aleissa BM. Prevalence of Temporomandibular Disorders Between 2015-2021: A Literature Review. Cureus 2023;15:e37028. doi: 10.7759/cureus.37028</ref>.
| |
| | |
| Diversi approcci terapeutici sono in fase di studio per la gestione dei TMD, con l'obiettivo di alleviare il dolore e migliorare la funzionalità della mandibola<ref>Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res 2018;11:571-87. doi: 10.2147/JPR.S127950</ref>. Sebbene siano disponibili metodi chirurgici e non chirurgici per trattare i TMD, il trattamento conservativo è l'opzione iniziale e primaria<ref>Abouelhuda AM, Khalifa AK, Kim YK, Hegazy SA. Non-invasive different modalities of treatment for temporomandibular disorders: review of literature. J Korean Assoc Oral Maxillofac Surg 2018;44:43-51. doi: 10.5125/jkaoms.2018.44.2.43</ref>. Le terapie farmacologiche comprendono l'uso di farmaci antinfiammatori non steroidei (FANS), antidepressivi e miorilassanti. Un'altra componente del trattamento consiste in tecniche di terapia occlusale e fisica, come la laserterapia a basso livello (LLLT) e la Stimolazione Elettrica Transcutanea del nervo trigeminale (TENS).<ref>Rezazadeh F, Hajian K, Shahidi S, Piroozi S. Comparison of the Effects of Transcutaneous Electrical Nerve Stimulation and Low-Level Laser Therapy on Drug-Resistant Temporomandibular Disorders. J Dent (Shiraz) 2017;18:187-92</ref>
| |
| | |
| La 'TENS' ha acquisito riconoscimento come tecnica non invasiva e priva di farmaci per la gestione del dolore nei TMD. Consiste nell'applicazione di correnti elettriche a bassa frequenza sulla pelle tramite elettrodi di superficie<ref>Shanavas M, Chatra L, Shenai P, Rao PK, Jagathish V, Kumar SP, et al. Transcutaneous electrical nerve stimulation therapy: An adjuvant pain controlling modality in TMD patients - A clinical study. Dent Res J (Isfahan) 2014;11:676-9</ref><ref>Martimbianco ALC, Porfírio GJ, Pacheco RL, Torloni MR, Riera R. Transcutaneous electrical nerve stimulation (TENS) for chronic neck pain. Cochrane Database Syst Rev 2019;12:CD011927. doi: 10.1002/14651858.CD011927.pub2</ref>. Queste correnti stimolano '''i nervi sensoriali''' e '''modulano i segnali del dolore''' trasmessi al sistema nervoso centrale (CNS), alterando la percezione del dolore. La TENS è utilizzata nei pazienti con TMD per mirare ai muscoli e ai nervi circostanti la TMJ, promuovendo il rilassamento muscolare, riducendo gli '''spasmi muscolari''' e alleviando il disagio<ref>Hsieh YL, Yang CC, Yang NP. Ultra-Low Frequency Transcutaneous Electrical Nerve Stimulation on Pain Modulation in a Rat Model with Myogenous Temporomandibular Dysfunction. Int J Mol Sci 2021;22:9906. doi: 10.3390/ijms22189906</ref>.
| |
| | |
| Comprendere l'efficacia comparativa della TENS e degli analgesici nel trattamento dei TMD è cruciale per i professionisti sanitari<ref>Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res 2018;11:571-87. doi: 10.2147/JPR.S127950</ref>. Identificando i vantaggi e gli svantaggi di entrambi gli approcci, i clinici possono selezionare l'opzione di trattamento più appropriata per ciascun paziente<ref>Beutler LE, Someah K, Kimpara S, Miller K. Selecting the most appropriate treatment for each patient. Int J Clin Health Psychol 2016;16:99-10. doi: 10.1016/j.ijchp.2015.08.001</ref>.
| |
| | |
| Confrontando la TENS con altre modalità di trattamento, studi hanno valutato la sua efficacia, sicurezza e praticabilità nel ridurre il dolore e '''migliorare la funzione''' masticatoria nei pazienti con TMD<ref>Chellappa D, Thirupathy M. Comparative efficacy of low-Level laser and TENS in the symptomatic relief of temporomandibular joint disorders: A randomized clinical trial. Indian J Dent Res 2020;31:42-7. doi: 10.4103/ijdr.IJDR_735_18</ref>.
| |
| | |
| Nonostante il crescente riconoscimento della TENS come approccio non invasivo per la gestione dei TMD, manca un'analisi comparativa completa della sua efficacia rispetto agli analgesici comunemente usati nel trattamento dei TMD<ref>Wu M, Cai J, Yu Y, Hu S, Wang Y, Wu M. Therapeutic Agents for the Treatment of Temporomandibular Joint Disorders: Progress and Perspective. Front Pharmacol 2021;11:596099. doi: 10.3389/fphar.2020.596099</ref>.
| |
| | |
| In letteratura possiamo evidenziare alcuni articoli degni di nota come quelli di:
| |
| | |
| * Rémi Esclassan<ref>Rémi Esclassan 1, Anaïs Rumerio 2, Paul Monsarrat 1 2, Jean Claude Combadazou 1 2, Jean Champion 1 2, Florent Destruhaut 1 2, Christophe Ghrenassia 1 2. Optimal duration of ultra low frequency-transcutaneous electrical nerve stimulation (ULF-TENS) therapy for muscular relaxation in neuromuscular occlusion: A preliminary clinical study. Cranio. . 2017 May;35(3):175-179.
| |
| | |
| doi: 10.1080/08869634.2016.1171479. Epub 2016 Apr 8.
| |
| </ref> del 2017 il cui obiettivo principale è stato quello di determinare la durata dell'applicazione della stimolazione elettrica transcutanea a frequenza ultra-bassa (ULF-TENS) necessaria per ottenere un sufficiente '''rilassamento dei muscoli masticatori'''. Nel complesso, i risultati suggeriscono che un'applicazione ideale di ULF-TENS dovrebbe durare 40 minuti per ottenere un rilassamento muscolare sufficiente sia nei pazienti con disturbi del sistema masticatorio '''sia nei soggetti sani''', una durata che risulta coerente con la pratica clinica quotidiana.
| |
| | |
| <blockquote>
| |
| La perplessità che sorge è capire quando e perchè un muscolo di un soggetto sano debba essere in una condizione di non rilassamento ed ottenerlo soltanto dopo TENS. Questo è il primo evidente fenomeno non ben chiaro che balza agli occhi e cioè la condizione di 'Tono muscolare'</blockquote>
| |
| | |
| * Rafaella Mariana Fontes de Bragança<ref>Rafaella Mariana Fontes de Bragança 1, Carolina Almeida Rodrigues 1, Melissa Oliveira Melchior 1, Laís Valencise Magri 1, Marcelo Oliveira Mazzetto 1. Ultra-low frequency transcutaneous electric nerve stimulation does not affect the centric relation registration. Cranio. . 2018 Jan;36(1):19-28.
| |
| | |
| doi: 10.1080/08869634.2016.1278107. Epub 2017 Jan 27.
| |
| </ref>del 2018 il cui obiettivo è stato quello di valutare l'influenza della ULF-TENS sullo spostamento del condilo mandibolare e sulla ripetibilità della registrazione della relazione centrica (CR) La ULF-TENS non ha influenzato lo spostamento totale del condilo, indipendentemente dalla tecnica di registrazione della CR utilizzata La tecnica 'bimanuale' ha mostrato un miglioramento nella ripetibilità dopo l'uso della ULF-TENS.
| |
| <blockquote>
| |
| La perplessità che sorge dalla lettura di questo articolo è perchè mai la TENS debba migliorare la ripetibilità della manovra centrica bimanuale forse la continui stimoli afferenti ai nuclei mesencefalici determinano una sorta di perdita delle stereognosica della mandbola. Allora dovremmo capire il funzionamento della TENs a livello neurofisiologico sia periferico che centrale, cosa che nei prossimi capitoli affronteremo. </blockquote>
| |
| | |
| * Yuanxiu Zhang<ref>Yuanxiu Zhang 1 2 3 4, Jinglu Zhang 1 3, Lin Wang 1 2 3, Kelun Wang 3 5, Peter Svensson 4 6 7. Effect of transcutaneous electrical nerve stimulation on jaw movement-evoked pain in patients with TMJ disc displacement without reduction and healthy controls. Acta Odontol Scand. . 2020 May;78(4):309-320.
| |
| | |
| doi: 10.1080/00016357.2019.1707868. Epub 2019 Dec 26.
| |
| </ref> del 2020 il cui obiettivo è stato quello di valutare l'effetto della TENS sul dolore e sui modelli di movimento dopo movimenti ripetuti della mandibola in pazienti con articolazioni temporomandibolari (TMJ) dolorose e spostamento del disco senza riduzione (DDwoR), e confrontarlii con volontari sani. I risultati hanno indicato che il dolore evocato dai movimenti è stato ridotto spontaneamente o dal sTENS nei pazienti con dolore alla TMJ con DDwoR e, in modo interessante, che la TENS potrebbe attenuare il dolore evocato dai movimenti e migliorare la funzione motoria della mandibola durante i movimenti ripetuti. I risultati potrebbero avere implicazioni per il trattamento con TENS nei pazienti con dolore alla TMJ con DDwoR.
| |
| | |
| <blockquote>
| |
| Anche qui la perplessità si focalizza sul meccanismo d'azione e cioè è una sorta di fenomeno di 'gate Control' oppure esclusivamente motorio? </blockquote>
| |
| | |
| * Syeda Mahnoor Fatima<ref>Syeda Mahnoor Fatima, Tooba Zahoor, Ramsha Nawaz, Ahmed Tanveer, Syeda Soveba Zaidi. Role of transcutaneous electrical nerve stimulation in temporomandibular joint disorders. J Pak Med Assoc. . 2024 Sep;74(9):1645-1648. doi: 10.47391/JPMA.10874.
| |
| </ref>molto recente del 2024 che partivano da un dato epidemiologico sconcertante e cioè che i loro risultati attuali erano coerenti con uno studio secondo cui il 5-60% della popolazione generale soffre di almeno uno dei segni del TMD. Inoltre, il 48% dei pazienti con TMD ha mostrato sintomi clinici, tra cui tenerezza muscolare e difficoltà ad aprire la bocca<ref>Ryan J, Akhter R, Hassan N, Hilton G, Wickham J, Ibarag S. Epidemiology of Temporomandibular Disorder in the General Population: a systematic review. Adv Dent & Oral Health 2019;10:555787. DOI: 10.19080/ADOH.2019.10.555787</ref>. Uno dei sottogruppi trattati con stimolazione nervosa elettrica a microcorrente (MENS) ha dimostrato un significativo miglioramento nei punteggi VAS.<ref>Saranya B, Ahmed J, Shenoy N, Ongole R, Sujir N, Natarajan S. Comparison of Transcutaneous Electric Nerve Stimulation (TENS) and Microcurrent Nerve Stimulation (MENS) in the Management of Masticatory Muscle Pain: A Comparative Study. Pain Res Manag 2019;2019:8291624. doi: 10.1155/2019/8291624</ref>
| |
| | |
| <blockquote>Qui la perplessità sta nel dato sconcertante del 60% dii popolazione che accusa Disturbi della ATM con rigidità muscolare e/o ridotta apertura della bocca, I casi in questo caso non sono infini ma solo due e cioè che sull'intera popolazione mondiale di 8 miliardi di persone 4 mliardi e 800 milioni di persone soffrono di Disordini Temporomandibolari? Forse stiamo perdendo il controllo del dato clinico e della valutazione clinica. Siamo sicuri di avere conoscenza e mezzi validi per interpretare lo stato di malattia di un soggetto TMDs? Dai capitoli precedntemente esposti nella sezione 'Scienza Normale' non sembra comunque approfondiamo il tema per capire semmai esista una anomalia nel sistema.</blockquote>Ancor più sconcertante è che un recentissimo articolo di Taseef Hasan Farook<ref>Taseef Hasan Farook, Tashreque Mohammed Haq, Lameesa Ramees, James Dudley. Predictive modelling of freeway space utilising clinical history, normalised muscle activity, dental occlusion, and mandibular movement analysis. SCI Rep</ref>pubblicato nel 2024 sulla rivista Scientific reports facente parte della prestigioso Nature Publishing Group arriva alle seguenti asserzioni.
| |
| | |
| IIl "freeway space" è la distanza tra le arcate dentarie in posizione di riposo<ref>Pleasure, M. A. Correct vertical dimension and freeway space. J Am Dental Assoc 43, 160–163 (1951)</ref>. È un parametro essenziale in protesi dentale, influenzando occlusione e dimensione verticale<ref>Pleasure, M. A. Correct vertical dimension and freeway space. J Am Dental Assoc 43, 160–163 (1951)</ref>. Un adeguato spazio interocclusale garantisce la stabilità protesica e previene disturbi temporomandibolari (TMD) e affaticamento muscolare<ref>Farook, T. H., Rashid, F., Alam, M. K. & Dudley, J. Variables influencing the device-dependent approaches in digitally analysing jaw movement—a systematic review. Clin. Oral. Investig. 27(2), 489–504 (2022)</ref>. Il TENS (Stimolazione Nervosa Elettrica Transcutanea) è utilizzato per rilassare i muscoli e valutare la corretta dimensione verticale in relazione allo spazio interocclusale<ref>Snyder, B., TENS and the treatment of TMJ dysfunction. J Prosthet Dent 45, 335–338 (1981)</ref>. Tecnologie recenti, come il deep learning, riducono la soggettività nelle misurazioni, standardizzando l'approccio clinico<ref>Farook, T. H. & Dudley, J. Automation and deep (machine) learning in temporomandibular joint disorder radiomics. A Systematic review. J. Oral. Rehabil. 50(6), 501–521 (2023)</ref>.
| |
| | |
| | |
| | |
| | |
| {| class="wikitable" | |
| |+
| |
| | colspan="5" |'''Table 1:''' DTM diagnostic methodologies analyzed and eliminated from the DRC because they are not scientifically validated
| |
| |-
| |
| |'''Diagnostic Tests'''
| |
| |'''Cutoff'''
| |
| |'''Sensitivity'''
| |
| |'''Specificity'''
| |
| |'''VPP'''
| |
| |-
| |
| | colspan="5" |'''Electrical stimulation methods'''
| |
| |-
| |
| |Free rest space before stimulation''( Cooper e Rabuzzi 1984)''<ref name=":1">BC Cooper, D D Rabuzzi. Myofacial pain dysfunction syndrome: a clinical study of asymptomatic subjects. Laryngoscope. 1984 Jan;94(1):68-75. doi: 10.1002/lary.5540940116.
| |
| </ref>
| |
| |0.75-2.0 mm
| |
| | 0.42
| |
| |0.62
| |
| |0.17
| |
| |-
| |
| |Free space to rest after electric-stimulation ''( Cooper e Rabuzzi 1984;''<ref name=":1" />)
| |
| |0.75-2.0 mm
| |
| |0.76
| |
| |0.19
| |
| |0.11
| |
| |-
| |
| |Closure trajectory before after electrical stimulation''( Cooper e Rabuzzi 1984)''<ref name=":1" />
| |
| |Non definita
| |
| |0.75
| |
| |0.27
| |
| |0.12
| |
| |-
| |
| | colspan="5" |<small>Cutoff: Parameters and limits of significance that should divide sick from healthy, for each test reported</small><small>Sensitivity: Ability of the specified test to identify the truly sick in a sample of healthy and sick subjects</small>
| |
| | |
| <small>Specificity: Ability of the specified test to identify the healthy in a sample of healthy and sick subjects</small>
| |
| | |
| <small>Positive Predictive Value (PPV): Ratio of the ability of the specified test to identify truly sick (positive) patients on the total sick population in a sample of healthy and sick subjects.</small>
| |
| |}
| |
| | |
| | |
| <references />
| |

 Change language
Change language

[[|German]]

[[|Spanish]]

[[|French]]

[[|Italian]]
Transcutaneous Electric Nerve Stimulation
In this chapter, we consider another highly debated topic: Transcutaneous Electrical Nerve Stimulation (TENS), on which there is still no unanimous opinion within the International Scientific Community. This premise is confirmed by the fact that, although the Research Diagnostic Criteria (RDC) have categorically invalidated the clinical procedure in diagnosing patients with Temporomandibular Disorders, the procedure is still considered valid. It continues to be discussed, articles are published, and it is still practiced. This inconsistency is demonstrated by scientific papers in the literature with intermediate and ambiguous conclusions, which generate only questions without providing valid answers.
The RDC has clinically deemed the TENS procedure invalid based on the freeway space and myocentric trajectory, both as diagnostic elements for Temporomandibular Disorders (TMD) and as part of masticatory prosthetic rehabilitation treatment. As can be seen from the specific section of Table 1 presented in the chapter Research Diagnostic Criteria (RDC), it is clear that both freeway space and TENS trajectory were excluded due to a low predictive value (PPV: 0.17). While this might be true, it is essential to delve into the technical and methodological details to understand the rationale behind this decision. For this reason, we will briefly but thoroughly describe the TENS method to better understand its weaknesses and strengths.
TENS and Temporomandibular Disorders: The temporomandibular joint (TMJ) is a hinge joint with biarticular properties, enabling the complex movements required for chewing. Temporomandibular disorder (TMD) occurs when the TMJ and associated anatomical structures are affected. Approximately 25% of individuals worldwide show signs or symptoms of TMD. TMD occurs 1.5 to 2.5 times more frequently in women than in men.
Various therapeutic approaches are being studied for managing TMD, aiming to relieve pain and improve jaw function. Although surgical and non-surgical methods are available for treating TMD, conservative treatment is the initial and primary option. Pharmacological therapies include the use of nonsteroidal anti-inflammatory drugs (NSAIDs), antidepressants, and muscle relaxants. Another treatment component consists of occlusal and physical therapy techniques, such as low-level laser therapy (LLLT) and Transcutaneous Electrical Nerve Stimulation of the trigeminal nerve (TENS).
TENS has gained recognition as a non-invasive and drug-free technique for pain management in TMD. It involves applying low-frequency electrical currents to the skin through surface electrodes. These currents stimulate sensory nerves and modulate pain signals transmitted to the central nervous system (CNS), altering pain perception. TENS is used in TMD patients to target muscles and nerves surrounding the TMJ, promoting muscle relaxation, reducing muscle spasms, and relieving discomfort.
.
Conclusion: Despite the controversy surrounding TENS in the treatment of TMD, studies show varying degrees of efficacy in pain reduction and muscle relaxation. However, its role compared to other treatment modalities remains unclear and requires further research to establish its definitive clinical utility.
To read the full text of this chapter, log in or request an account
A Google Account is needeed to request a Member Account