The logic of classical language -print
Classical logic will be discussed in this chapter. In the first part, mathematical formalism and the rules that compose it will be illustrated. In the second part, a clinical example will be given to evaluate its effectiveness in determining a diagnosis.
In conclusion, it is evident that a classical logic of language, which has an extremely dichotomous approach (either something is white, or it is black), cannot describe the many shades that real clinical situations have.
As we shall soon see, this paper will show that classical logic lacks the necessary precision, forcing us to enhance it with other types of logic languages.
Introduction
We parted ways in the previous chapter on the ‘Logic of Medical Language’ in an attempt to shift the attention from clinical symptom or sign to encrypted machine language for which, the arguments of Donald E Stanley, Daniel G Campos and Pat Croskerry are welcome but connected to time Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle t_n}
as an information carrier (anticipation of the symptom) and to the message as a machine language and not as a non-verbal language).[1][2]
Obviously, this does not preclude the validity of the clinical history built on a pseudo-formal verbal language by now well rooted in the clinical reality and which has already proved its diagnostic authority. The attempt to shift attention to a machine language and to the System provides nothing but an opportunity for the validation of Diagnostic Medical Science.
We are definitely aware that our Linux Sapiens is still perplexed about what has been anticipated and continues to wonder.
«... but... could the logic of Classical Language help us to solve poor Mary Poppins' dilemma?»
(a little patience, please) |
We cannot provide a conventional answer because science does not progress with assertions that are not justified by scientifically validated questions and reflections; and this is actually the reason why we will try to give voice to some thoughts, perplexities and doubts expressed on some basic topics brought into discussion in some scientific articles.
One of these fundamental topics is 'Craniofacial Biology'.
Let's start with a well known study by Townsend and Brook[3]: in this work the authors question the status quo of both fundamental and applied research in 'Craniofacial Biology' to extract clinical considerations and implications. One topic they covered was the "Interdisciplinary Approach", in which Geoffrey Sperber and his son Steven saw the strength of the exponential progress of 'Craniofacial Biology' in technological innovations such as gene sequencing, CT scanning, MRI imaging, scanning laser, image analysis, ultrasonography and spectroscopy[4].
Another topic of great interest for the implementation of 'Craniofacial Biology' is the awareness that biological systems are 'Complex Systems'[5] and that 'Epigenetics' plays a key role in craniofacial molecular biology. Researchers from Adelaide and Sydney provide a critical review in the field of epigenetics aimed, in fact, at the dental and craniofacial disciplines.[6] Phenomics, in particular, discussed by these authors (see Phenomics)) is a general research field that involves the measurement of changes in the teeth and associated orofacial structures resulting from the interactions between genetic, epigenetic and environmental factors during development.[7] In this same context, the work of Irma Thesleff from Helsinki, Finland, should be highlighted. She explains in her work that there are a series of transient signalling centres in the dental epithelium that play important roles in the programme of tooth development.[8] Besides there are other works, by Peterkova R, Hovor akova M, Peterka M, Lesot H, providing a fascinating review of the processes that occur during dental development;[9][10][11] for the sake of completeness, let's not forget the works by Han J, Menicanin D, Gronthos S, and Bartold PM., who review comprehensive documentation on stem cells, tissue engineering and periodontal regeneration.[12]
In this review, arguments could not be missing on genetic, epigenetic and environmental influences during morphogenesis that lead to variations in the number, size and shape of the tooth[13][14] and the influence of tongue pressure on growth and craniofacial function.[15][16]Townsend and Brook's extraordinary work too deserves a mention[3], and the intrinsic content of what has been reported in it matches equally well with another commendable author: HC Slavkin.[17] Slavkin asserts that:
- "The future is full of significant opportunities to improve the clinical outcomes of congenital and acquired craniofacial malformations. Clinicians play a key role as critical thinking and clinical audience substantially improve diagnostic accuracy and therefore clinical health outcomes."
«I understand the progress of Science described by the authors but I don't understand the change of thought»
(I'll give you a practical example) |
In the chapter "Introduction" we posed certain questions on the subject of malocclusion but in this context we simulate the dentist's logic of medical language when faced with the clinical case presented in the "Introduction chapter" with its diagnostic and therapeutic conclusions.
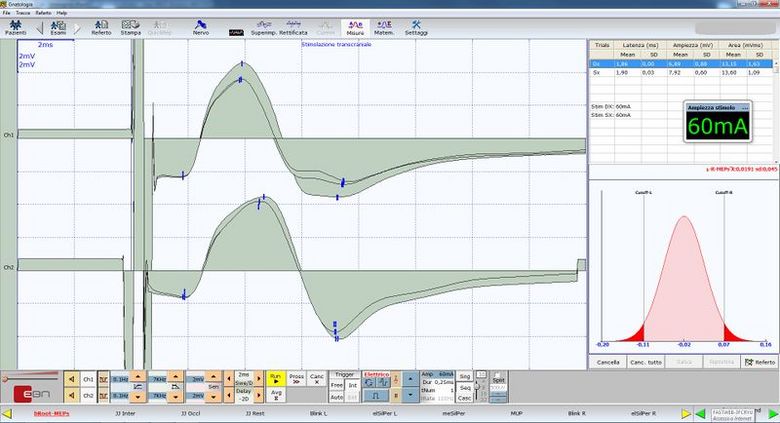
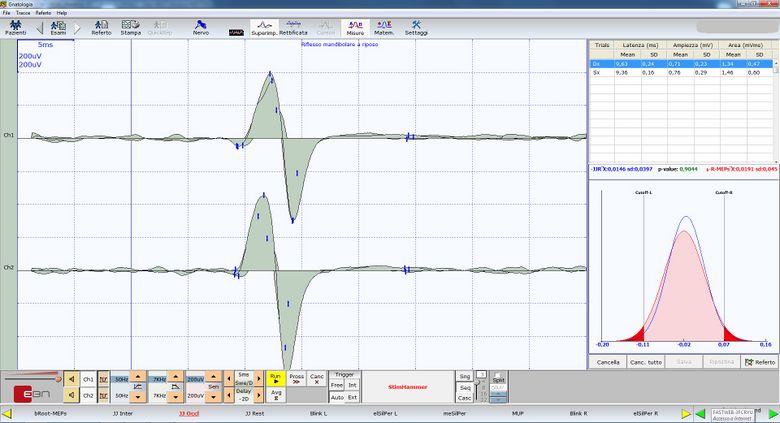
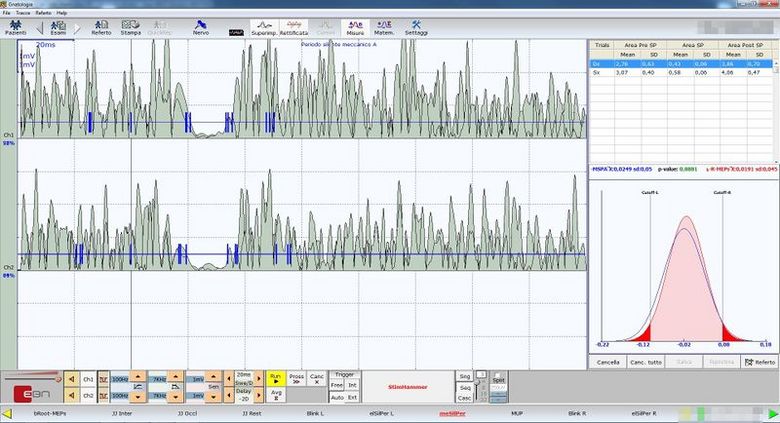
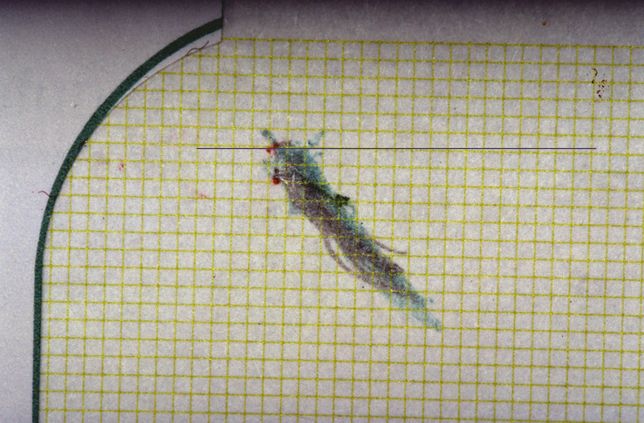
The patient has a posterior unilateral crossbite and an anterior openbite.[18] The crossbite is another disturbing element of the normal occlusion[19] for which it is compulsorily treated together with the openbite.[20][21] This type of reasoning means that the model (masticatory system) is 'normalized to occlusion'; and read in reverse, it means that the occlusal discrepancy is the cause of malocclusion, hence, a disease of the Masticatory System, and therefore an intervention to restore the physiological masticatory function is justifiable. (Figure 1a).
This example is Classical Logic Language, as we are going to explain in detail, but now a doubt arises:
- At the time when orthodontic and orthognathics axioms were constructing protocols confirmed by the International Scientific Community, were they aware of the information we discussed in the introduction to this chapter?
Certainly not because time Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle t_n} is the bearer of information but despite this cognitive limit we proceed with a very questionable Classical Language Logic for the safety of the citizen.
«... this statement seems a bit risky!»
(sure, but the logical sequence has already been anticipated) |
If the same case were interpreted with a mindset that followed a 'System's language logic' (it will be discussed in the appropriate chapter), the conclusions would be surprising.
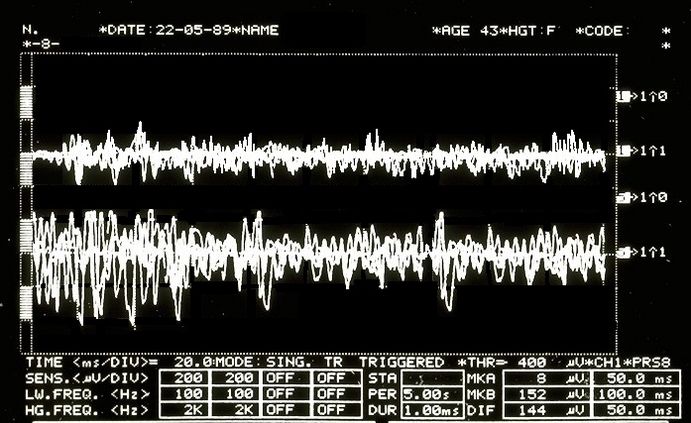
If we observe the electrophysiological responses performed on the patient with malocclusion in figures 1b, 1c and 1d (with the explanation made directly in the caption to simplify the discussion), we shall notice that these data can make us think about anything except a 'Malocclusion' and, therefore, the axioms of type orthodontic and orthognathics 'cause/effect' leave a conceptual void.
«Let me better understand what Classical Language Logic has to do with it»
(We will do it following the clinical case of our Mary Poppins) |
Mathematical formalism
In this chapter, we will reconsider the clinical case of the unfortunate Mary Poppins suffering from Orofacial Pain for more than 10 years to which her dentist diagnosed a 'Temporomandibular Disorders' (TMDs) or rather Orofacial Pain from TMDs. To better understand why the exact diagnostic formulation remains complex with a Logic of Classical Language, we should understand the concept on which the philosophy of classical language is based with a brief introduction to the topic.
Propositions
Classical logic is based on propositions. It is often said that a proposition is a sentence that asks whether the proposition is true or false. Indeed, a proposition in mathematics is usually either true or false, but this is obviously a little too vague to be a definition. It can be taken, at best, as a warning: if a sentence, expressed in common language, makes no sense to ask whether it is true or false, it will not be a proposition but something else.
It can be argued whether or not common language sentences are propositions as in many cases it is not often evident if a certain statement is true or false.
Fortunately, mathematical propositions, if well expressed, do not show such ambiguities’.
Simpler propositions can be combined with each other to form new, more complex propositions. This occurs with the help of operators called logical operators and quantifying connectives which can be reduced to the following[22]:
- Conjunction, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \land} (and):
- Disjunction, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \lor} (or):
- Negation, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \urcorner} (not):
- Implication, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Rightarrow} (if ... then):
- Consequence, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \vdash} (is a partition of..):
- Universal quantifier, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \forall} (for all):
- Demonstration, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \mid} (such that): and
- Membership, which is indicated by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \in} (is an element of) or by the symbol Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \not\in} (is not an element of):
Demonstration by absurdity
Furthermore, in classical logic there is a principle called the excluded third which declares that a sentence that cannot be false must be taken as true since there is no third possibility.
Suppose we need to prove that the proposition Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle p} is true. The procedure consists in showing that the assumption that Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle p} is false leads to a logical contradiction. Thus the proposition Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle p} cannot be false, and therefore, according to the law of the excluded third, it must be true. This method of demonstration is called demonstration by absurdity[23]
Predicates
What we have briefly described so far is the logic of propositions. A proposition asserts something about specific mathematical objects such as: '2 is greater than 1, so 1 is less than 2' or 'a square has no 5 sides then a square is not a pentagon'. Many times, however, the mathematical statements concern not the single object, but generic objects of a set such as: 'Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle X} are taller than 2 meters' where Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle X} denotes a generic group (for example all volleyball players). In this case we speak of predicates.
Intuitively, a predicate is a sentence concerning a group of elements (which in our medical case will be the patients) and which states something about them.«Then poor Mary Poppins is a TMD patient or she is not!»
(let's see what Classical Language Logic tells us) |
2nd Clinical Approach
Dental propositions
While seeking to use the mathematical formalism to translate the conclusions reached by the dentist with classical logic language, we consider the following predicates:
- x Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \equiv} Normal patients (normal stands for patients commonly present in the specialist setting)
- Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle A(x) \equiv} Bone remodelling with osteophyte from stratigraphic examination and condylar CT; and
- Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle B(x)\equiv} Temporomandibular Disorders (TMDs) resulting in Orofacial Pain (OP)
- Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \mathrm{a}\equiv} Specific patient: Mary Poppins
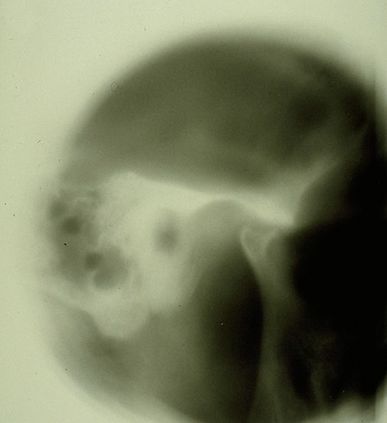
Any normal patient Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \forall\text{x} } who is positive on the radiographic examination of the TMJ Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \mathrm{\mathcal{A}}(\text{x})} [Figure 2 and 3] is affected by TMDs Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \rightarrow\mathrm{\mathcal{B}}(\text{x})} ; from this it follows that Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \vdash} being Mary Poppins positive (and also being a "Normal" patient) on the TMJ x-ray Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle A(a)} then Mary Poppins is also affected by TMDs Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \rightarrow \mathcal{B}(a)} The language of predicates is expressed in the following way:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \{a \in x \mid \forall \text{x} \; A(\text{x}) \rightarrow {B}(\text{x}) \vdash A( a)\rightarrow B(a) \}} . Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (1)}
At this point, it must also be considered that predicate logic is not used only to prove that a particular set of premises imply a particular evidence Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (1)} . It is also used to prove that a particular assertion is not true, or that a particular piece of knowledge is logically compatible/incompatible with a particular evidence.
In order to prove that this proposition is true we must use the above mentioneddemonstration by absurdity. If its denial creates a contradiction, surely the dentist's proposition will be true:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \urcorner\{a \in x \mid \forall \text{x} \; A(\text{x}) \rightarrow {B}(\text{x}) \vdash A( a)\rightarrow B(a) \}} . Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (2)}
"Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (2)} " states that it is not true that those who test positive on TMJ CT have TMDs, so Mary Poppins (TMJ CT positive normal patient) does not have TMDs.
The dentist believes that Mary Poppins' claim (that she does not have TMD under these premises) is a contradiction so the main claim is true.
Neurophysiological proposition
Let us imagine that the neurologist disagrees with the conclusion Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (1)} and asserts that Mary Poppins is not affected by TMDs or that at least it is not the main cause of Orofacial Pain, but that, rather, she is affected by a neuromotor Orofacial Pain (nOP), therefore that she does not belong to the group of 'normal patients' but is to be considered a 'non-specific patient' (uncommon in the specialist context).
Obviously, this dialectic would last indefinitely because both would defend their scientific-clinical context; but let us see what happens in the logic of predicates.
The neurologist's statement would be like:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \{a \not\in x \mid \forall \text{x} \; A(\text{x}) \rightarrow {B}(\text{x}) \and A( a)\rightarrow \urcorner B(a) \}} . Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (3)}
"Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (3)} " means that every patient with CT positive of TMJ could not be TMDs.
In order to prove that this proposition is true, we must use once again the above mentioned demonstration by absurdity. If its denial creates a contradiction, surely the neurologist's proposition will be true:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \urcorner\{a \not\in x \mid \forall \text{x} \; A(\text{x}) \rightarrow {B}(\text{x}) \and A( a)\rightarrow \urcorner B(a) \}} . Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (4)}
Following the logical rules of predicates, there is no reason to say that denial (4) is contradictory or meaningless, therefore the neurologist (unlike the dentist) would not seem to have the logical tools to confirm his conclusion.«then the dentist triumphs!»
(don't take it for granted) |
Compatibility and incompatibility of the statements
The complication lies in the fact that the dentist will present a series of statements as clinical reports such as the stratigraphy and CT of the TMJ, that indicate an anatomical flattening of the joint, axiography of the condylar traces with a reduction in kinematic convexity and a tracing EMG interference pattern in which an asymmetrical pattern on the masseters is highlighted. These assertions can easily be considered a contributing cause of the damage to the Temporomandibular Joint and, therefore, responsible for the 'Orofacial pain'.
Documents, reports and clinical evidence can be used to make the neurologist's assertion incompatible and the dentist's diagnostic conclusion compatible. To do this we must present some logical rules that describe the compatibility or incompatibility of the logic of classical language:
- A set of sentences Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im} , and a number Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle n\geq1} of other phrases or statements Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (\delta_1,\delta_2,.....\delta_n \ )} are logically compatible if, and only if, the union between them Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im\cup\{\delta_1,\delta_2.....\delta_n\}} is coherent.
- A set of sentences Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im} , and a number Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle n\geq1} of other phrases or statements Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (\delta_1,\delta_2,.....\delta_n \ )} are logically incompatible if, and only if, the union between them Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im\cup\{\delta_1,\delta_2.....\delta_n\}} is incoherent.
Let us try to follow this reasoning with practical examples:
The dentist colleague exposes the following sentence:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im} : Following the personalized techniques suggested by Xin Liang et al.[28] who focuses on the quantitative microstructural analysis of the fraction of the bone value, the trabecular number, the trabecular thickness and the trabecular separation on each slice of the CT scan of a TMJ, it appears that Mary Poppins is affected by Temporomandibular Disorders (TMDs) and the consequence causes Orofacial Pain.
At this point, however, the thesis must be confirmed with further clinical and laboratory tests, and in fact the colleague produces a series of assertions that should pass the compatibility filter as described above, namely:
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \delta_1=} Bone remodelling: The flattening of the axiographic traces highlighted in figure 5 indicates the joint remodelling of the right TMJ of Mary Poppins, such a report can be correlated to a series of researches and articles that confirm how malocclusion can be associated with morphological changes in the temporomandibular joints, particularly when combined with the age as the presence of a chronic malocclusion can worsen the picture of bone remodelling.[29] These scientific references determine the compatibility of the assertion.
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \delta_2=} Sensitivity and specificity of the axiographic measurement: A study was conducted to verify the sensitivity and specificity of the data collected from a group of patients affected by temporomandibular joint disorders with an ARCUSdigma axiographic system[30]; it confirmed a sensitivity of the 84.21% and a 92.86% sensitivity for the right and left TMJs respectively, and a specificity of 93.75% and 95.65%.[31] These scientific references determine compatibility of the assertion in the dental context precisely because of the consistency of related studies.[32]
Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \delta_3=} Alteration of condylar paths: Urbano Santana-Mora and coll.[33] evaluated 24 adult patients suffering from severe chronic unilateral pain diagnosed as Temporomandibular Disorders (TMDs). The following functional and dynamic factors were evaluated:
masticatory function; remodelling of the TMJ or condylar pathway (CP) and lateral movement of the jaw or lateral guide (LG).
The CPs were assessed using conventional axiography and LG was assessed by using kinesiograph tracing[34]; Seventeen (71%) of the 24 (100%) patients consistently showed a side of habitual chewing side. The mean and standard deviation of the CP angles was 47.90 9.24) degrees. The average of LG angles was 42.9511.78 degrees.
Data collection emerged from the conception of a new TMD paradigm in which the affected side could be the usual chewing side, the side where the mandibular lateral kinematic angle was flatter. This parameter may also be compatible with the dental claim.
EMG Intereference pattern: M.O. Mazzetto and coll.[35] showed that the electromyographic activity of the anterior temporal muscles and the masseter was positively correlated with the "Craniomandibular index", indiced (CMI) with a and suggesting that the use of CMI to quantify the severity of TMDs and EMG to assess the masticatory muscle function, may be an important diagnostic and therapeutic elements. These scientific references determine compatibility of the assertion.
?
Obviously, the dentist colleague could endlessly keep on casting his statements, indefinitely.
Well, all of these statements seem coherent with the sentence initially described, whereby the dentist colleague feels justified in saying that the set of sentences , and a number of other assertions or clinical data Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (\delta_1,\delta_2,.....\delta_n \ )} are logically compatible as the union between them Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im\cup\{\delta_1,\delta_2.....\delta_n\}} is coherent.«Following the logic of classical language, the dentist is right!»
(It would seem so! But, be careful, only in his own dental context!) |
This statement is so true that the Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle P-value}
could be infinitely extended, widened enough to obtain an Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \alpha=0}
that corresponds to it in an infinite significance, as long as it remains limited in its context; yet, without meaning anything from a clinical point of view in other contexts, like in the neurologist one, for instance.
Final considerations
From a perspective of observation of this kind, the Logic of Predicates can only fortify the dentist’s reasoning and, at the same time, strengthen the principle of the excluded third: the principle is strengthened through the compatibility of the additional assertions Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (\delta_1,\delta_2,.....\delta_n \ )} which grant the dentist a complete coherence in the diagnosis and in confirming the sentence Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im} : Poor Mary Poppins either has TMD, or she has not.«...and what if, with the advancement of research, new phenomena were discovered that would prove the neurologist right, instead of the dentist?»
|
Basically, given the compatibility of the assertions , coherently saying that Orofacial Pain is caused by a Temporomandibular Disorders could become incompatible if another series of assertions Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle (\gamma_1,\gamma_2,.....\gamma_n \ )}
were shown to be coherent: this would make a different sentence compatible Failed to parse (MathML with SVG or PNG fallback (recommended for modern browsers and accessibility tools): Invalid response ("Math extension cannot connect to Restbase.") from server "https://wikimedia.org/api/rest_v1/":): {\displaystyle \Im}
: could poor Mary Poppins suffer from Orofacial Pain from a neuromotor disorder (nOP) and not by a Temporomandibular Disorders?
In the current medical language logic, such assertions only remain assertions, because the convictions and opinions do not allow a consequent and quick change of the mindset.
Moreover, taking into account the risk that this change entails, in fact, we might consider a recent article on the epidemiology of temporomandibular disorders[36] in which the authors confirm that despite the methodological and population differences, pain in the temporomandibular region appears to be relatively common, occurring in about the 10% of the population; we may then objectively be led to hypothesize that our Mary Poppins can be included in the 10% of the patients mentioned in the epidemiological study, and contextually be classified as a patient suffering from Orofacial Pain from Temporomandibular Disorders (TMDs).
In conclusion, it is evident that a classical logic of language, which has an extremely dichotomous approach (either it is white or it is black), cannot depict the many shades that occur in real clinical situations.
We need to find a more convenient and suitable language logic...«... can we then think of a Probabilistic Language Logic?»
(perhaps) |
- ↑ Stanley DE, Campos DG, «The logic of medical diagnosis», in Perspect Biol Med, 2013».
PMID:23974509
DOI:10.1353/pbm.2013.0019 - ↑ Croskerry P, «Adaptive expertise in medical decision making», in Med Teach, 2018».
PMID:30033794
DOI:10.1080/0142159X.2018.1484898 - ↑ 3.0 3.1 Townsend GC, Brook AH, «The face, the future, and dental practice: how research in craniofacial biology will influence patient care», in Aust Dent J, Australian Dental Association, 2014».
PMID:24646132
DOI:10.1111/adj.12157 - ↑ Sperber GH, Sperber SM, «The genesis of craniofacial biology as a health science discipline», in Aust Dent J, Australian Dental Association, 2014».
PMID:24495071
DOI:10.1111/adj.12131 - ↑ Brook AH, Brook O'Donnell M, Hone A, Hart E, Hughes TE, Smith RN, Townsend GC, «General and craniofacial development are complex adaptive processes influenced by diversity», in Aust Dent J, Australian Dental Association, 2014».
PMID:24617813
DOI:10.1111/adj.12158 - ↑ Williams SD, Hughes TE, Adler CJ, Brook AH, Townsend GC, «Epigenetics: a new frontier in dentistry», in Aust Dent J, Australian Dental Association, 2014».
PMID:24611746
DOI:10.1111/adj.12155 - ↑ Yong R, Ranjitkar S, Townsend GC, Brook AH, Smith RN, Evans AR, Hughes TE, Lekkas D, «Dental phenomics: advancing genotype to phenotype correlations in craniofacial research», in Aust Dent J, Australian Dental Association, 2014».
PMID:24611797
DOI:10.1111/adj.12156 - ↑ Thesleff I, «Current understanding of the process of tooth formation: transfer from the laboratory to the clinic», in Aust Dent J, 2013».
DOI:10.1111/adj.12102 - ↑ Peterkova R, Hovorakova M, Peterka M, Lesot H, «Three‐dimensional analysis of the early development of the dentition», in Aust Dent J, Wiley Publishing Asia Pty Ltd on behalf of Australian Dental Association, 2014».
DOI:10.1111/adj.12130 - ↑ Lesot H, Hovorakova M, Peterka M, Peterkova R, «Three‐dimensional analysis of molar development in the mouse from the cap to bell stage», in Aust Dent J, 2014».
DOI:10.1111/adj.12132 - ↑ Hughes TE, Townsend GC, Pinkerton SK, Bockmann MR, Seow WK, Brook AH, Richards LC, Mihailidis S, Ranjitkar S, Lekkas D, «The teeth and faces of twins: providing insights into dentofacial development and oral health for practising oral health professionals», in Aust Dent J, 2013».
DOI:10.1111/adj.12101 - ↑ Han J, Menicanin D, Gronthos S, Bartold PM, «Stem cells, tissue engineering and periodontal regeneration», in Aust Dent J, 2013».
DOI:10.1111/adj.12100 - ↑ {{Cite book | autore = Brook AH | autore2 = Jernvall J | autore3 = Smith RN | autore4 = Hughes TE | autore5 = Townsend GC | titolo = The Dentition: The Outcomes of Morphogenesis Leading to Variations of Tooth Number, Size and Shape | url = https://onlinelibrary.wiley.com/doi/epdf/10.1111/adj.12160 | volume = | opera = Aust Dent J | anno = 2014 | editore = | città = | PMID = | PMCID = | DOI = 10.1111/adj.12160 | oaf = | LCCN = | OCLC =
- ↑ Seow WK, «Developmental defects of enamel and dentine: challenges for basic science research and clinical management», in Aust Dent J, 2014».
PMID:24164394
DOI:10.1111/adj.12104 - ↑ Kieser JA, Farland MG, Jack H, Farella M, Wang Y, Rohrle O, «The role of oral soft tissues in swallowing function: what can tongue pressure tell us?», in Aust Dent J, 2013».
DOI:10.1111/adj.12103 - ↑ Slavkin HC, «Research on Craniofacial Genetics and Developmental Biology: Implications for the Future of Academic Dentistry», in J Dent Educ, 1983».
PMID:6573384 - ↑ Slavkin HC, «The Future of Research in Craniofacial Biology and What This Will Mean for Oral Health Professional Education and Clinical Practice», in Aust Dent J, 2014».
PMID:24433547
DOI:10.1111/adj.12105 - ↑
Littlewood SJ, Kandasamy S, Huang G, «Retention and relapse in clinical practice», in Aust Dent J, 2017».
DOI:10.1111/adj.12475 - ↑ Miamoto CB, Silva Marques L, Abreu LG, Paiva SM, «Impact of two early treatment protocols for anterior dental crossbite on children’s quality of life», in Dental Press J Orthod, 2018».
- ↑ Alachioti XS, Dimopoulou E, Vlasakidou A, Athanasiou AE, «Amelogenesis imperfecta and anterior open bite: Etiological, classification, clinical and management interrelationships», in J Orthod Sci, 2014».
DOI:10.4103/2278-0203.127547 - ↑ Mizrahi E, «A review of anterior open bite», in Br J Orthod, 1978».
PMID:284793
DOI:10.1179/bjo.5.1.21 - ↑ For the sake of simplicity of exposition and reading, we will deal in this chapter with the symbol of belonging, the symbol of consequence and the "such that" as if they were quantifiers and connectives of propositions in classical logic.
Strictly speaking, within classical logic they should not be treated as such, but even if we do, this does not absolutely change the meaning of the speech and no inconsistencies of any kind are created. - ↑ Pereira LM, Pinto AM, «Reductio ad Absurdum Argumentation in Normal Logic Programs», Arg NMR, 2007, Tempe, Arizona - Caparica, Portugal – in «Argumentation and Non-Monotonic Reasoning - An LPNMR Workshop».
- ↑ Castroflorio T, Talpone F, Deregibus A, Piancino MG, Bracco P, «Effects of a Functional Appliance on Masticatory Muscles of Young Adults Suffering From Muscle-Related Temporomandibular Disorder», in J Oral Rehabil, 2004».
PMID:15189308
DOI:10.1111/j.1365-2842.2004.01274.x - ↑ Maeda N, Kodama N, Manda Y, Kawakami S, Oki K, Minagi S, «Characteristics of Grouped Discharge Waveforms Observed in Long-term Masseter Muscle Electromyographic Recording: A Preliminary Study», in Acta Med Okayama, Okayama University Medical School, 2019, Okayama, Japan».
PMID:31439959
DOI:10.18926/AMO/56938 - ↑ Rudy TE, «Psychophysiological Assessment in Chronic Orofacial Pain», in Anesth Prog, American Dental Society of Anesthesiology, 1990».
ISSN: 0003-3006/90
PMID:2085203 - PMCID:PMC2190318 - ↑ Woźniak K, Piątkowska D, Lipski M, Mehr K, «Surface electromyography in orthodontics - a literature review», in Med Sci Monit, 2013».
e-ISSN: 1643-3750
PMID:23722255 - PMCID:PMC3673808
DOI:10.12659/MSM.883927 - ↑ Liang X, Liu S, Qu X, Wang Z, Zheng J, Xie X, Ma G, Zhang Z, Ma X, «Evaluation of Trabecular Structure Changes in Osteoarthritis of the Temporomandibular Joint With Cone Beam Computed Tomography Imaging», in Oral Surg Oral Med Oral Pathol Oral Radiol, 2017».
PMID:28732700
DOI:10.1016/j.oooo.2017.05.514 - ↑ Solberg WK, Bibb CA, Nordström BB, Hansson TL, «Malocclusion Associated With Temporomandibular Joint Changes in Young Adults at Autopsy», in Am J Orthod, 1986».
PMID:3457531
DOI:10.1016/0002-9416(86)90055-2 - ↑ KaVo Dental GmbH, Biberach / Ris
- ↑ Kobs G, Didziulyte A, Kirlys R, Stacevicius M, «Reliability of ARCUSdigma (KaVo) in Diagnosing Temporomandibular Joint Pathology», in Stomatologija, 2007».
PMID:17637527 - ↑ Piancino MG, Roberi L, Frongia G, Reverdito M, Slavicek R, Bracco P, «Computerized axiography in TMD patients before and after therapy with 'function generating bites'», in J Oral Rehabil, 2008».
PMID:18197841
DOI:10.1111/j.1365-2842.2007.01815.x - ↑ López-Cedrún J, Santana-Mora U, Pombo M, Pérez Del Palomar A, Alonso De la Peña V, Mora MJ, Santana U, «Jaw Biodynamic Data for 24 Patients With Chronic Unilateral Temporomandibular Disorder», in Sci Data, 2017».
PMID:29112190 - PMCID:PMC5674825
DOI:10.1038/sdata.2017.168
This is an Open Access resource! - ↑ Myotronics Inc., Kent, WA, US
- ↑ Oliveira Mazzetto M, Almeida Rodrigues C, Valencise Magri L, Oliveira Melchior M, Paiva G, «Severity of TMD Related to Age, Sex and Electromyographic Analysis», in Braz Dent J, 2014».
DOI:10.1590/0103-6440201302310 - ↑ LeResche L, «Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors», in Crit Rev Oral Biol Med, 1997».
PMID:9260045
DOI:10.1177/10454411970080030401