Logique du système
Ce chapitre ferme la boucle de la « Logique du langage médical » pour introduire un modèle de diagnostic dans le domaine des fonctions masticatoires qui combine la conceptualité de la logique des systèmes avec la mécanique quantique. Les modèles mathématiques statistiques d'une logique de système ne peuvent donc pas être subjectifs, ni approximatifs, encore moins vagues et non formels dans le contexte du modèle clinique. Pour obtenir ces caractéristiques, il est nécessaire de considérer les concepts de base de la « théorie des systèmes ».
La percée diagnostique irréfutable dans la plupart des disciplines médicales réside dans la bio-ingénierie, les progrès technologiques et plus particulièrement la théorie des systèmes. Il permet de vérifier l'état d'un système en comparant les variables de sortie générées par les variables d'entrée. Ce grand pas en avant réside dans l’introduction du concept de déclencheur. La bio-ingénierie dans le contexte électrophysiologique du trijumeau a permis l'utilisation d'une série de déclencheurs (stimulation électrique transcrânienne, stimulation magnétique transcrânienne, stimulation mécanique du district du trijumeau) qui nous permettent de tester le système avec une résolution beaucoup plus élevée que celle dans laquelle le système est testé. sans répondre à un déclencheur externe. Un autre élément clé est que le modèle de déclenchement est capable de fournir un instantané de l’état du système plusieurs années avant l’apparition d’un signe clinique pathologique évident.
Dans ce chapitre, nous expliquerons quelques étapes de base à suivre pour modéliser les méthodes de diagnostic selon la théorie des systèmes.
Article by Gianni Frisardi · Giorgio Cruccu · Alice Bisirri · Pier Paolo Valentini · Flavio Frisardi · Irene Minciacchi
|
Avant-propos
Pourquoi en sommes-nous arrivés à la « logique système » ? Les étapes ne sont ni triviales, ni personnelles, et pour percevoir la valeur ajoutée de la « Logique Système » on ne peut s'empêcher de mentionner deux raisons essentielles qui ont jalonné ce chemin : celle des indices cliniques dentaires et de la logique du langage médical.
Index cliniques dentaires
Il existe des « indices » qui peuvent être considérés comme des éléments de la logique système en tant que données objectives, tels que « l'équation de Henderson-Hasselbalch » (pour l'analyse du pH sanguin) et d'autres « indices » développés dans le domaine médical dans des disciplines disparates.[1][2][3]
Un test, une donnée de référence normative ou un « Indice » (ainsi qu'une « Constante ») sont des stratégies liées aux modèles mathématiques-statistiques qui génèrent des données. Ces données sont obligatoires pour l'exactitude du diagnostic, pour le diagnostic différentiel ainsi que pour les orientations thérapeutiques. Sur ces données de référence, au cours de l'histoire scientifique de la dentisterie, des implémentations et des modifications ont été générées, mais aussi des incertitudes et des croyances qui, sous forme d'axiomes ou d'écoles de pensée, ont fixé des lignes directrices qui ne sont pas toujours scientifiquement justifiables et parfois fausses.
Dans la littérature
Nous pouvons prendre en considération les données rapportées dans la littérature concernant les « Indices » étudiés sur des patients souffrant de 'Troubles temporo-mandibulaires'[4] ou entrer plus spécifiquement dans les réhabilitations masticatoires et vérifier le thème « Indices cliniques » dans les disciplines orthodontiques.[5]
Dans un article récent d'Andrea Scribante et collaborateurs,[6] par exemple, les paragraphes suivants sont déduits :
- L'introduction indique que l'évaluation des résultats du traitement orthodontique est traditionnellement réalisée en utilisant l'expérience et les opinions subjectives des cliniciens.[7] Dans ce premier paragraphe, la limite du concept exprimé est comprise et le fait qu'un test diagnostique et/ou une ligne directrice thérapeutique ne doit jamais être scientifiquement évalué à l'aide de paramètres subjectifs.
- Cependant, depuis les années 1990, des indices spécifiques ont été développés pour évaluer objectivement les résultats en matière de santé en analysant la qualité des traitements.[8] Ces indices comparent les données avant et après traitement pour déterminer le résultat du traitement orthodontique[9] et améliorer la qualité des traitements futurs.[10] Ce deuxième paragraphe scientifiquement acceptable met en évidence le but des « Indices » et c'est la comparaison avant et après - mais qui a dit que le poste est en état de « normocclusion » et le pré en « malocclusion », l'alignement dentaire ?
- L'indice le plus couramment utilisé pour évaluer le succès orthodontique est l'indice d'évaluation par les pairs (PAR), qui a été développé pour mesurer dans quelle mesure un patient s'écarte de l'occlusion et de l'alignement normaux.[8] Cet indice a été utilisé pour évaluer les effets de la thérapie dans différentes circonstances: l'utilisation d'appareils fixes et mobiles,[11] la comparaison des traitements orthodontiques entre cabinets privés et écoles d'orthodontie,[12] l'évaluation de la stabilité occlusale après un traitement orthodontique,[13] les traitements précoces[14] et les résultats de la chirurgie orthognathique.[15] Nous devons considérer que le PAR n'indiquerait pas le sain ou le malade, la normocclusion ou la malocclusion selon qu'il s'éloigne du seuil, mais face à une série de caractéristiques entrantes, il renverrait une réponse à large spectre (Index), valable pour traitements orthodontiques et orthognathiques. Cet état d'esprit est légitime mais les cliniciens doivent être prudents car les variables d'entrée (les « Constructeurs ») du modèle ou de l'entrée peuvent ne pas être liées au contexte de référence ou il peut y avoir d'autres variables cachées qui invalideraient le résultat lui-même. . Nous apprécierons plus fortement ces affirmations dans l’exposé des chapitres de Masticationpedia.
The fact is that the primum movens of the studio of Andrea Scribante and collaborators is concentrated in the following point:
(Limitative .... the index can have an accuracy and truthfulness in dental alignment but not to validate a normocclusion, this latter assertion is much more complex to formulate and certainly cannot be reduced exclusively to an 'Occlusal observable'.)
Spyridon N. Papageorgiou[16] in a very interesting study exposes a corageous statement that confirms what has just been exposed:
- Noticeable long-term occlusal changes are observed in the post-debond, which mostly favor better settlement. The higher quality finish at the debond significantly influenced the possibilities for improvement. However, setting a cutoff score to denote treatment excellence has shown considerable instability over time.
Other authors state that relapse after orthodontic treatment can also occur in cases with good functional occlusion.[17]
Further considerations
The etiology of recurrence is neither fully understood nor can it be fully predicted from a single factor,[18] but includes factors such as the response of the traction and deconstructed periodontal fibers,[19] physiological maturation of the human dentition which affects its width, length or perimeter[20], alterations of the craniofacial complex[21] and parafunctions.[22]
Retention of treatment results is therefore considered to be one of the most difficult problems in orthodontics, and relapses, especially of the mandibular incisors, could also be observed with the use of retention devices after debonding.[23] Most of the existing post-treatment stability studies evaluate short-term relapses of the anterior region by primarily measuring the irregularity of the incisors after extractive or non-extractive treatment and compare different retention patterns. These studies largely use the Peer Assessment Rating (PAR) index[24] which is not a trigeminal electrophysiological analysis approach in considering 'Normocclusion' much less the details of a well balanced occlusion (such as contacts, inclinations and alignment of each tooth) or changes in retention only in the short term.[25]
To the authors' knowledge at the time of publication of their study, only one study[26] used the American Board of Orthodontics (ABO)[27] detailed objective classification system for models and radiographs which measures the details of a well-finished and well-balanced occlusion.
(Constructive criticism, however, is inherent in the statement itself: how is an efficient masticatory function and, therefore, a 'Normocclusion' defined?)
In Masticationpedia, we would like to launch interesting and constructive provocations to answer the question we just set out: 'How is an efficient chewing function and therefore a Normocclusion defined?'
Let's look at the two cases below, in figure 1 and in figure 2: which of the two clinical cases do you think is affected by malocclusion?
It seems irreverent for the canons of orthodox orthodoxy not to share the diagnosis of 'malocclusion', but we leave the reader in a little suspense. We intend to resume extensively in a few chapters, after deepening the topic of 'System Logic' and 'Systems Theory'. We only anticipate that the patient in figure 1 has already been proposed in the chapter 'Introduction', so we already know our clinical scientific opinion but if he gives us so much, also.....
(... be patient and you will see)
Medical language logic
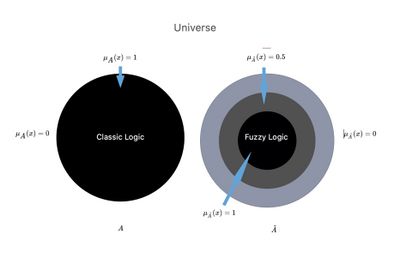
In the previous chapters we highlighted the extreme difficulties we met in defining an exact, detailed and timely diagnosis in the right time; and this is not only due to the 'Complexity' of the living system, but also to a questionable and vague logic of medical language. If classical logic is too selective (true or false, and therefore 'there is no third answer' - principle of the excluded third), it is also true that probabilistic logic language, which trivially indicates the presence of a specific disease, breaks down in the 'significativity' parameter that acquires a certain value only in a 'specialist context'.
We perceived the need for a more elastic model called "fuzzy logic" that could translate the uncertainty inherent in some human language data into mathematical formalism, codifying the "elastic" concepts (such as almost high, fairly good, etc), in order to make them understandable and manageable by computers.
We have therefore frozen a much debated and approached concept in the chapter 'Introduction': not determining a clear separation between specialist know-how, but superimposing interdisciplinary knowledge, instead, through a 'Fuzzy' approach (see fuzzy logic language).
Systems Theory
In the scientific field, systems theory, more properly general system theory (definition by Ludwig von Bertalanffy),[28] is an often interdisciplinary field of study, straddling mathematics and natural sciences, which deals with the analysis of properties and the constitution of a system. It is essentially composed of the theory of dynamic systems (simple and complex) and of the theory of control: it is the basis of various disciplines such as automation, robotics and cybernetic physics, as well as the technical-scientific study of systems in general as much as in biology and medicine.
Systems theory is the interdisciplinary study of systems, that could be described as cohesive groups of interconnected and interdependent parts that can be natural or man-made. Each system is bounded by space and time, influenced by its environment, defined by its structure and expressed through its functioning. A system can be more than the sum of its parts if it expresses emerging synergies or behaviors.[29]
Changing one part of a system might affect other parts or the whole system. It may be possible to predict these changes in behavior patterns. Some systems support other systems, keeping the others to prevent failure. The goals of systems theory are to model the dynamics, constraints, conditions of a system and to clarify the principles (such as purpose, measure, methods, tools) that can be identified and applied to other systems at any level of nesting and in a 'wide range of fields to achieve optimized equifinality.[30]
To be practical and effective in the description of the concept 'System logic' we consider an approach to a part of the trigeminal motor system, since it is the cornerstone of this scientific work, in which the conceptual connection with the 'Theory of Systems'.
Masticatory System Logic
Regarding the analysis of the state of the masticatory system, the EMG technique has been widely used but there are still a number of concerns regarding the reliability of the measures based on the interferential EMG. [31]
This is why most of the studies performed so far aimed at showing a possible correlation between EMG signals with Temporomandibular Disorders (TMD), Orofacial Pain (OP) or Malocclusion (IO), but they have not yielded convincing results.[32]
In an unknown percentage of OP patients visited by specialist dentists, some neurological diseases such as intracranial tumours, multiple sclerosis, etc. are the underlying symptoms cause of TMD or OP.
These patients, who actually suffer from neurological symptoms superimposed on dental-facial ones, may undergo unnecessary dental interventions before the correct diagnosis is made, sometimes too late.[33]
(... as said, the 'Observable' cannot be the occlusal element because it is hierarchically lower than the Trigeminal Nervous System.)
Cortical projections to the trigeminal motor neurons are generally believed to be bilateral and symmetrical and can be electrophysiologically analyzed by electrical or magnetic brain stimulation through the intact scalp.[34]
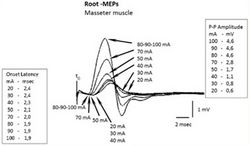
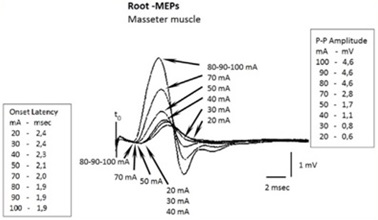
In the ipsilateral masseter, the transcranial electrical stimulation (eTCS) is capable of evoking a large short-latency potential in relaxed and active muscles. The characteristics of ipsilateral Motor Evoked Potentials (MEPs) do not change under relaxed or active conditions. Mean onset latency is approximately 2 ms, peak latency of 3.9 ms and amplitude of 5.4 mV, and there is no latency variability in similar pacing conditions. These motor potentials, considered secondary to trigeminal motor root excitation, have been called Root-MEP (Root-MEP or simplified into R-MEPs) to differentiate them from M-waves and Cortex-MEPs.[35]
To make the understanding of 'Systems Theory' more suitable for the context of the masticatory system, we report some trigeminal electrophysiological procedures and implement them with the mathematical models of the theory.
Mathematical formalism in 'Systems Theory'
The "systems theory" studies oriented systems, in which it becomes possible to classify the quantities of interest into two categories:
- quantities that vary over time independently from the others (inputs)
- quantities whose evolution over time is to be studied, depending on the inputs, called outputs.
A real system can have multiple inputs and multiple outputs. In particular, we indicate with:
- the vector of the inputs at time
- the vector of the output at time
It is also generally defined as the state vector of the system in a generic instant the information instantly necessary to uniquely determine the output for each once the entrance has been assigned .
We denote the state vector, whose components are defined as state variables, with the notation .
The inputs act on the state of the system and modify its characteristics at a given moment in time; these changes are recorded by the state variables. The values of the system outputs, usually the only measurable variables, in turn depend on the system state variables and the inputs.
The input, status and output quantities are functions of the time variable.
This takes values in an ordered subset , which can be continuous or discrete. In the following discussion we will consider a discrete subset of times:
Therefore, given a set of times , we can formally define a system as the pair of equations
with , where is called generating function e is called the output transformation.
In the field of biosignals, the () models are used to analyze EEG and vibration systems in vehicles, human hearing systems and vascular systems, and so on. While much is still unknown about the physiological mechanism or pattern of internal changes in the tested system, the output transfer or transformation function in our context allows us to reconstruct a wave function by interpolating the points detected by the instrument which has its own particular sampling frequency. This function, for our purposes, is a reconstruction of a wave function on which to search for latencies, amplitudes and integral areas and make the necessary conclusions,[36][37] and, obviously, by retesting the system in subsequent epochs, the integrity of the system itself can be compared.
In the engineering field, various mathematical modeling of a system are possible, depending on whether or not they explicitly consider the state variables.
Mathematical formalism of the Trigeminal System Logic
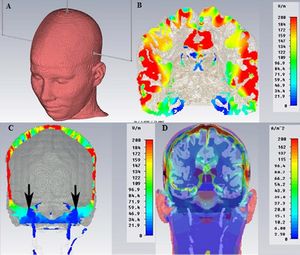
We consider the Trigeminal Motor System as a black box with inputs (figure 5) and outputs (figure 6), and we try to adapt to it the above described theory.
Figure 6 shows the neuromotor responses to the electrical transcranial stimulation of the trigeminal root of the right hemilate. We wanted to set up the test following the mathematical model of 'systems theory' to better understand the difference between the information obtained from a now almost inflated test such as the interferential EMG, and a more complex test such as a motor and/or somatosensory evoked potential; the evoked potential has the prerogative of a system response to an external input called 'trigger', which in this context is of an electrical type.
We divided the test by delivering a series of progressively greater electrical stimuli in the ordered times corresponding to.
In our context, we will have one input, i.e. the electrical stimulation amperage and two outputs, i.e. latency and amplitude.
We will therefore have:
mA.
Two state variables will correspond to each of these inputs: latency and amplitude .
ms
mV
All these variables generate a plotting of multiple mediated traces as in figure 6, in which some important considerations can be made, such as the decrease in latency and the increase in amplitude as the amperage increases.
Conclusion
It is plausible that the reader, or a colleague not accustomed to particular trigeminal electrophysiological procedures, may consider this type of bioengineering diagnostic models exaggerated, both for the difficulty in the execution (that can make the methodology seem dangerous - the Root-MEPs delivers an electric current of 100 V with an amperage of 100mA), and for the feeling he might have that the cost benefit is unjustified; so, he might prefer to continue with the now routine methodology in dentistry, such as performing a simple, fast and inexpensive interferential EMG (Figure 7A). We certainly accept the opinion of our hypothetical colleague, but we do not share it because, to save a human life, competence is always and critically required, together with dedication and both intellectual and economic investment.
The irrefutable step forward made in diagnostics in most medical disciplines, as already mentioned, lies precisely in bioengineering, technological progress; specifically, systems theory has allowed us to verify the system state by comparing output variables generated by variables incoming payments which are basically triggers of various types.
Figure 7 is a way of demonstrating this. Notably, like the interferential EMG test shows (Figure 7A), only a sort of interferential asymmetry typical of clinical situations of malocclusion can be observed, while through a trigger model (specifically, the bilateral transcranial electrical stimulation of the trigeminal roots) the system responds with a large amplitude asymmetry (Figure 7B) and even with an absence of the jaw jerk response (evoked with a mechanical trigger by striking the chin with a neurological piezoelectric hammer). (Figure 7C) The diagnostic conclusion of this patient was of skull base menygoma.
For the experts, of course, a glance is enough to understand whether the trigeminal motor system evoked through electrical transcranial stimulation of the motor roots is in a physiological or pathological state; but, as we will see in the next chapters, the biological reality is so complex and paradoxically indeterministic, that a bioengineering model paired with an adequate statistical mathematician will allow us to approach more accurately the real physiopathological state of the system, reduce the uncertainty of the measurement and consequently the differential diagnostic error but above all make early diagnosis.
In any case, if this patient had undergone the described diagnostic model, he would not have died, because the growth of the tumor mass of a meningioma is extraencephalic, and slow, and would have shown an electrophysiologically documentable destructuring many years before the vertiginous symptomatology.(see: 3° Clinical case: Meningioma )
- ↑ Wei Xiao, Yi Yang, Jiao Shi, Jia Xu, Jianguang Zhu, Zhinong Wu, «The diagnostic efficacy and predictive value of combined lipoprotein laboratory indexes for atherosclerosis», in J Pak Med Assoc, 2020».
PMID:33177739 - ↑ Diana Ferraro, Roberta Bedin, Patrizia Natali, Diego Franciotta, Krzysztof Smolik, Mario Santangelo, Paolo Immovilli, Valentina Camera, Francesca Vitetta, Matteo Gastaldi, Tommaso Trenti, Stefano Meletti, Patrizia Sola, «Kappa Index versus CSF Oligoclonal Bands in Predicting Multiple Sclerosis and Infectious/Inflammatory CNS Disorders», in Diagnostics (Basel), MDPI, 2020».
PMID:33096861 - PMCID:PMC7589948
DOI:10.3390/diagnostics10100856
This is an Open Access resource! - ↑ Huseyin Kayadibi, Baris Yilmaz, Abdullah Ozgur Yeniova, Huseyin Koseoglu, Zahide Simsek, «Development and evaluation of a novel noninvasive index for predicting significant fibrosis, advanced fibrosis, and cirrhosis in patients with chronic hepatitis B infection», in Eur J Gastroenterol Hepatol., 2021».
PMID:33177385
DOI:10.1097/MEG.0000000000001973 - ↑ Results in PubMed for "Temporomandibular disorders Index"
- ↑ Results in PubMed for "Orthodontics Indexes"
- ↑ Maria Francesca Sfondrini, Paolo Zampetti, Giulia Luscher, Paola Gandini, José Luís Gandía-Franco, Andrea Scribante, «Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating)», in Healthcare (Basel), MDPI, 2020».
PMID:33182796 - PMCID:PMC7711869
DOI:10.3390/healthcare8040473.
This is an Open Access resource! - ↑ Dyken RA, Sadowsky PL, Hurst D, «Orthodontic outcomes assessment using the peer assessment rating index», in Angle Orthod, The EH Angle Education and Research Foundation, Inc., 2001».
PMID:11407767
DOI:<0164:OOAUTP>2.0.CO;2 10.1043/0003-3219(2001)071<0164:OOAUTP>2.0.CO;2 - ↑ 8.0 8.1 Richmond S, Shaw WC, O’Brien KD, Buchanan IB, Jones R, Stephens CD, Roberts CT, Andrews M, «The development of the PAR Index (Peer Assessment Rating): reliability and validity», in Eur J Orthod, Oxford University Press, 1992, Oxford UK».
PMID:1582457
DOI:10.1093/ejo/14.2.125 - ↑ Onyeaso CO, BeGole EA, «Associations between pretreatment age and treatment time with orthodontic treatment outcome: A comparison by means of two orthodontic indices», in Hell Orthod. Rev, MDPI, 2008, Basel, Switzerland».
- see alsoThis is an Open Access resource! - ↑ Hickman JH, «Directional edgewise orthodontic approach. 5», in J Clin Orthod, 1975».
PMID:1054697 - ↑ Firestone AR, Häsler RU, Ingervall B, «Treatment results in dental school orthodontic patients in 1983 and 1993», in Angle Orthod, The Edward H. Angle Society of Orthodontists, Inc., 1997, Bern, Switzerland».
PMID:10022180
DOI:<0019:TRIDSO>2.3.CO;2 10.1043/0003-3219(1999)069<0019:TRIDSO>2.3.CO;2 - ↑ Cook DR, Harris EF, Vaden JL, «Comparison of university and private-practice orthodontic treatment outcomes with the American Board of Orthodontics objective grading system», in Am J Orthod Dentofacial Orthop».
PMID:15953896
DOI:10.1016/j.ajodo.2004.12.014 - ↑ Ramanathan C, «PAR index in the evaluation of the stability of the orthodontic treatment results. A review», in Acta Medica (Hradec Králové), 2006, Hradec Králové, Czech Republic».
PMID:17438831
DOI:10.14712/18059694.2017.133 - ↑ Pangrazio-Kulbersh V, Kaczynski R, Shunock M, «Early treatment outcome assessed by the Peer Assessment Rating index», in Am J Orthod Dentofacial Orthop, 1999».
PMID:10229887
DOI:10.1016/s0889-5406(99)70277-5 - ↑ Templeton KM, Powell R, Moore MB, Williams AC, Sandy R, «Are the Peer Assessment Rating Index and the Index of Treatment Complexity, Outcome, and Need suitable measures for orthognathic outcomes?», in Eur J Orthod, Oxford University Press on behalf of the European Orthodontics Society, 2006, Oxford UK».
PMID:16648208
DOI:10.1093/ejo/cji120 - ↑ Spyridon N. Papageorgiou, Theodore Eliades, Christine Angst, «Stability of occlusal outcome during long-term retention: the time-dependent variation of the American Board of Orthodontics index», in Eur J Orthod, Zurich Open Repository and Archive, University of Zurich, 2021, Zurich, Switzerland».
PMID:32144422
DOI:10.1093/ejo/cjaa004 - ↑ Nadia Lyotard, Mark Hans, Suchitra Nelson, Manish Valiathan, «Short-term postorthodontic changes in the absence of retention», in Angle Orthod, 2010».
PMID:20677953 - PMCID:PMC8929484
DOI:10.2319/010210-7.1 - ↑ Little RM, «Stability and relapse of dental arch alignment», in Br J Orthod., University of Washington, Seattle, 1990, Washington, USA».
PMID:2207055
DOI:10.1179/bjo.17.3.235 - ↑ Reitan K, Kvam E, «Comparative behavior of human and animal tissue during experimental tooth movement», in Angle Orthod, 1971».
PMID:4992550
DOI:<0001:CBOHAA>2.0.CO;2 10.1043/0003-3219(1971)041<0001:CBOHAA>2.0.CO;2 - ↑ Birgit Thilander, «Dentoalveolar development in subjects with normal occlusion. A longitudinal study between the ages of 5 and 31 years», in Eur J Orthod, Oxford University Press on behalf of the European Orthodontic Society, 2009, Göteborg, Sweden».
PMID:19304760
DOI:10.1093/ejo/cjn124 - ↑ Behrents RG, Harris EF, Vaden JL, Williams RA, Kemp DH, «Relapse of orthodontic treatment results: growth as an etiologic factor», in J Charles H. Tweed Int Found, 1989».
PMID:2634695 - ↑ Günter Lang, Günter Alfter, Gernot Göz, Günter H Lang, «Retention and stability--taking various treatment parameters into account», in J Orofac Orthop, 2002».
PMID:11974450
DOI:10.1007/s00056-002-0036-2 - ↑ Jeanett Steinnes, Gunn Johnsen, Heidi Kerosuo, «Stability of orthodontic treatment outcome in relation to retention status: An 8-year follow-up», in Am J Orthod Dentofacial Orthop, 2017».
PMID:28554448
DOI:10.1016/j.ajodo.2016.10.032 - ↑ Karina Maria Salvatore de Freitas, Guilherme Janson, Marcos Roberto de Freitas, Arnaldo Pinzan, José Fernando Castanha Henriques, Célia Regina Maio Pinzan-Vercelino, «Influence of the quality of the finished occlusion on postretention occlusal relapse», in Am J Orthod Dentofacial Orthop, 2007».
PMID:17920494
DOI:10.1016/j.ajodo.2007.02.051 de Freitas, K.M., Janson, G., de Freitas, M.R., et al. Influence of the quality of the finished occlusion on postretention occlusal relapse. American Journal of Orthodontics and Dentofacial Orthopedics, 132, 428.e9-14. - ↑ Hoybjerg, A.J., Currier, G.F., Kadioglu, O. Evaluation of 3 retention protocols using the American Board of Orthodontics cast and radiograph evaluation. American Journal of Orthodontics and Dentofacial Orthopedics, 2013, 144, 16-22.
- ↑ Nett, B.C., Huang, G.J.Long-term posttreatment changes measured by the American Board of Orthodontics objective grading system. American Journal of Orthodontics and Dentofacial Orthopedics, 2005, 127, 444-50.
- ↑ Casko, J.S., Vaden, J.L., Kokich, V.G., Damone, J., James, R.D., Cangialosi, T.J., Riolo, M.L., Owens, S.E. Jr and Bills, E.D. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics, 1998, 114, 589–599.
- ↑ Ludwig von Bertalanffy, «General System Theory: Foundations, Development, Applications», in Arch Gen Psychiatry, George Braziller, 1968, New York».
ISBN: 978-0807604533
DOI:10.1001/archpsyc.1969.01740200123021 - ↑ Emergent Behaviour
- ↑ Equifinality
- ↑ Reaz MB, Hussain MS, Mohd-Yasin F (2006) Techniques of EMG signal analysis: detection, processing, classification and applications (Correction). Biol Proced Online 8: 163.
- ↑ Masci C, Ciarrocchi I, Spadaro A, Necozione S, Marci MC, et al. (2013) Does orthodontic treatment provide a real functional improvement? A case control study. BMC Oral Health 13: 57.
- ↑ Moazzam AA, Habibian M, «Patients appearing to dental professionals with orofacial pain arising from intracranial tumors: a literature review», in Oral Surg Oral Med Oral Pathol Oral Radiol, 2012».
PMID:23036798
DOI:10.1016/j.oooo.2012.06.017 - ↑ Merton PA, Morton HB, «[1]», in Nature, Springer Nature Limited, 1980».
PMID:7374773
DOI:10.1038/285227a0 - ↑ Cruccu G, Berardelli A, Inghilleri M, Manfredi M, «Functional organization of the trigeminal motor system in man. A neurophysiological study», in Brain, 1989».
PMID:2804615
DOI:10.1093/brain/112.5.1333 - ↑ Haebeom L, Hyunho K, Jungkuk K, Hwan-Sup O, Young-Jae P, Young-Bae P, «Feasibility study of transfer function model on electrocardiogram change caused by acupuncture», in BMC Complement Altern Med, 2017».
PMID:28178964 - PMCID:PMC5299648
DOI:10.1186/s12906-017-1615-5
This is an Open Access resource! - ↑ Smith RJ, Kamali G, Hays M, Coogan C, Crone NE, Kang JY, Sarma SV, «Transfer Function Models for the Localization of Seizure Onset Zone From Cortico-Cortical Evoked Potentials», in Front Neurol, Frontiers in Neurology, 2020».
PMID:33362689 - PMCID:PMC7758451
DOI:10.3389/fneur.2020.579961
This is an Open Access resource!
particularly focusing on the field of the neurophysiology of the masticatory system