1° Caso clínico: Espasmo hemimasticatorio
En los capítulos anteriores hemos considerado la complejidad diagnóstica en medicina teniendo en cuenta especialmente algunos parámetros como las variables ocultas que sólo la evolución de los conocimientos básicos en el tiempo nos permitirán identificar y las dificultades para descifrar la señal cifrada que el Sistema Nervioso Central envía al exterior en forma de lenguaje verbal.
Por último, pero no menos importante, las limitaciones impuestas por una mentalidad determinista que reduce el conocimiento en contextos especializados al limitar su capacidad diagnóstica. Una mentalidad alternativa a la determinística que considere principalmente una lógica de lenguaje difuso y el importante aporte de la probabilidad cuántica nos permitiría ampliar los horizontes científico-clínicos y adentrarnos en una realidad mesoscópica.
En este capítulo, por tanto, abordaremos el diagnóstico de nuestra Mary Poppins siguiendo el proceso científico-clínico, evaluando las dificultades de implementación y el valor añadido del código cifrado identificado en la transmisión hepática.
Introducción
Por lo expuesto en los capítulos anteriores desde la 'Introducción' a los capítulos de 'Lógica del lenguaje médico', más allá de la complejidad de los argumentos y la vaguedad del lenguaje verbal, nos encontramos ante un dilema que del contexto en al que se remite a la paciente y en estos casos para nuestra pobre Mary Poppins parece dominar el contexto odontológico, dadas las afirmaciones positivas que reportan los exámenes clínicos y de laboratorio practicados a la paciente.
(parecería aparentemente pero ......)
El caso clínico de nuestra pobre Mary Poppins muestra toda la complejidad fisiopatológica y clínica pero sobre todo un fenómeno de superposición de proposiciones, enunciados y frases lógicas en el contexto odontológico y neurológico en el que un contexto obtiene compatibilidad y coherencia mientras que el otro incoherencia.
Básicamente, dada la compatibilidad y consistencia de la oración (contexto odontológico) con las aseveraciones derivadas del reporte del ensayo clínico , decir constantemente que el dolor orofacial es causado por un trastorno temporomandibular podría volverse incompatible si otro conjunto de declaraciones clínicas fueron consistentes con la oración (contexto neurológico) y contextualmente opuesto, desde un punto de vista diagnóstico, a
Por tanto, existiría una fuente de conflicto logístico entre los dos contextos especialistas con inevitable retraso diagnóstico, contaminando también el proceso de descifrado de la señal en el lenguaje máquina del Sistema Nervioso Central (SNC).
Lo que determinará la clave de acceso para decodificar el código encriptado en lenguaje máquina (SNC) y nos permitirá interceptar una línea de demarcación será un dato clínico y/o de laboratorio irrefutable llamado ,lo que confirmará o excluirá la consistencia de una afirmación que la otra. Es fundamental, en este punto, una sentencia (sentencia de demarcación) del tipo será:
¿Mary Poppins tiene un trastorno neuromotor o un trastorno temporomandibular?
Te explicamos este paso en detalle:
Recuerda que da 'La lógica del lenguaje clásico' esto demuestra:
- Un conjunto de oraciones, y un número de otros enunciados son lógicamente compatibles si, y sólo si, la unión entre ellos es consistente
- Un conjunto de oraciones, y un número de otros enunciados son lógicamente compatibles si, y sólo si, la unión entre ellos es inconsistente
Importancia de los contextos
Ahora bien, para el contexto odontológico tendremos las siguientes oraciones y afirmaciones a las cuales le damos un valor numérico para facilitar el tratamiento y es decir dónde indica 'normalidad' y 'anormalidad' y por lo tanto la positividad del informe:
Informe radiológico positivo de la ATM en la Figura 2, Anormalidad, positividad del informe
Informe de TC positivo de la ATM en la Figura 3, Anormalidad, positividad del informe
Informe axiográfico positivo de los trazos condilares en la Figura 4, Anormalidad, positividad del informe
Patrón de interferencia EMG asimétrico en la Figura 5, Anormalidad, positividad del informe
La frase (contexto dental) con un número De otros lógicamente compatibles aseveraciones determinan la unión y coherencia entre ellas y se representan con un formalismo matemático para facilitar la dialéctica diagnóstica de la siguiente forma:
que representa el promedio de las declaraciones individuales reportadas. La media se diseñó porque muchas veces puede pasar que algunas pruebas den respuestas negativas a las que dar el valor
El resultado en este caso es y al mismo tiempo deriva el enunciado coherente de la oración en el que se argumenta que la sintomatología de la paciente Mary Poppins está determinada por la presencia de una DTM.
(y es precisamente aquí donde los contextos entran en conflicto)
En el contexto neurológico, por tanto, tendremos las siguientes frases y afirmaciones a las que damos un valor numérico para facilitar el tratamiento y que es dónde indica 'normalidad' y 'anormalidad' y por lo tanto la positividad del informe:
Ausencia de reflejo mandibular en las Figuras 6, Anormalidad, positividad del informe
Ausencia del periodo maseterino silente en las Figuras 7, Anormalidad, positividad del informe
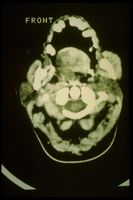
Hipertrofia del masetero derecho en la TC en las Figuras 8, Anormalidad, positividad del informe
Ahora, en consecuencia, también sentencia con un numero de otras sentencias lógicamente compatibles determinar la unión y coherencia entre ellos y la representación formal será similar a la del contexto odontológico:
con afirmación contextual coherente de oración en el que se argumenta que la sintomatología de la paciente Mary Poppins tiene una causa neuromotora y las consecuencias clínicas de tipo masticatorio oclusal no son otra cosa que consecuencia del daño neuropático.
Demarcator of coherence
The is a representative clinical specific weight, complex to research and fine-tune because it varies from discipline to discipline and for pathologies, essential in order not to make logical assertions collide and in the diagnostic procedures and essential to initialize the decryption of the logic communication code. Basically it allows you to confirm the consistency of a union with respect to another and vice versa, giving greater weight to the severity of the statements and the report in the appropriate context.
Sometimes the physician is faced with a series of positive reports to which to give due weight, he must consider the positivity of a report that highlights, for example, an osteoarticular remodeling of the TMJ cannot have the same weight as a positivity of a report confirming a latency delay of a trigeminal reflex.
The weight of demarcation , therefore, gives more significance to the most serious assertions in the clinical context from which they derive and therefore beyond the positivity of the or assertions which in any case are always verified and respected, these must be multiplied by a where indicates 'Low severity' while 'High severity'.
In the neurological context, concerns the presence of delays and/or latency absence of the jaw jerk, duration and/or absence of the masseterine silent period as well as other parameters that for the moment it is not necessary to describe. A delay greater than the normative value or an absence of the aforementioned tests is considered as a serious and absolute specific weight corresponding to a dominant valence with respect to the other clinical context.
To recap we therefore have:
where
average of the value of clinical statements in the dental context and therefore
average of the value of clinical statements in the neurological context and therefore
low severity performance of the dental contextreporting of high severity of the neurological context
where the 'coherence marker '' will define the diagnostic path as follows
Once we have washed away the myriad of positively reported normative data, which generate conflicts between contexts, thanks to the coherence marker we have a much clearer and more linear picture on which to deepen the analysis of the functionality of the Central Nervous System. Consequently we can concentrate on intercepting the tests necessary to decrypt the machine language code that the SNC sends out converted into verbal language.
Ephaptic transmission
With a little effort and patience on the part of passionate readers who have followed the entire logical path, sometimes apparently off topic, we have reached a clinical picture in which the code to be decrypted is inherent in neuromotor damage. Consequently, the access keys to the code, the one that figuratively corresponds to the exact decryption algorithm, would correspond to the right choice of the neuromotor damage detector test.
This is a point where it is essential to infer the clinician's intuition because finding the right algorithm to decrypt the code, after the aforementioned filter steps that have been described to wash away the interference of assertions, means at least choosing the right dictionary, for example, that of the image (MR of the brain rather than the neck); acoustic and vestibular evoked potentials (if a vestibular scwannoma is suspected) or trigeminal electrophysiological study (if more than one trigeminal involvement is suspected).
In this clinical iter that we have presented, the choice of the clinician to follow the electrophysiological trigeminal roadmap from which the positivity of the assertions have already been derived, therefore, having already defined a picture of serious anomaly of absence of the jaw jerk and of the silent period masseterino on the right side of the patient will have to understand if the damage is intracranial or extracranial.
To do this, the clinician uses an electrical stimulation test of the masseter nerve in infratemporal fossa called on the masseter muscle with simultaneous recording of the heteronymous on the temporal muscle[1] and a bilateral transcranial electrical stimulation of the trigeminal motor roots called, precisely, [2]
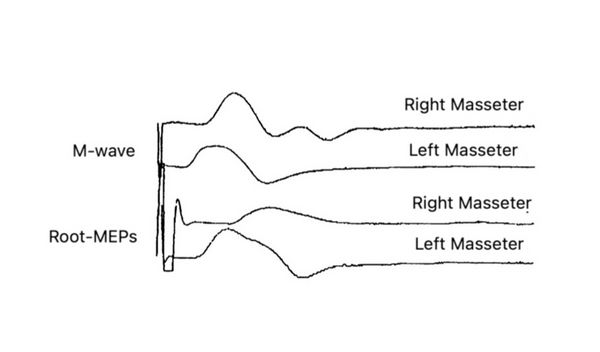
M-wave
The right masseter nerve was electrically stimulated in the infratemporal fossa (see clinical procedure chapter: Encrypted code: Ephaptic transmission) with a technique similar to that described by Macaluso & De Laat (1995).[3] Square cathode pulses (0.1 ms) generated by an electrical stimulator (Neuropack X1, Nihon Kohden Corporation, Tokyo, Japan) were delivered through a Teflon-coated monopolar needle electrode (TECA 902-DMG25, 53534) with a tip non-isolated (diameter 0.36 mm; area 0.28 mm2) inserted 1.5 cm through the skin below the zygomatic arch and anterior to the temporomandibular joint in the infratemporal fossa with electrical shocks of 0.5 - 5 mA, and 0.1 ms. The anode was a surface non-polarizable Ag-AgCl disc electrode (OD 9.0 mm) positioned over the ipsilateral ear lobe. Electrical stimulation of the masseter nerve never produced pain, and the subjects only perceived muscle contraction. The correct position of the stimulation electrodes was monitored throughout the experimental session by checking online the size of the M wave in the masseter muscle. The signals were recorded by placing surface electrodes on the masseter and temporal muscles and filtered at 10-2000Hz and by concentric needle electrodes inserted into the anterior temporal muscle.
bRoot-MEPs
The trigeminal root was stimulated transcrally through high voltage, low impedance through an electrical stimulator (Neuropack X1, Nihon Kohden Corporation, Tokyo, Japan)) with the anode electrode positioned at the apex and the cathode approximately 10 cm laterally from the apex along a line vertex acoustic meatus. The electric field is believed to excite the trigeminal motor nerve fibers via the trancranial route, near their exit from the skull.[2][4] Also in this case, the response in the right masseter was markedly delayed (3.5 ms on the right side 2 ms on the left and dispersed. amplitude of the M-wave.
Having highlighted, through the execution of the and test, a delay in the conduction speed of the trigeminal nerve fibers generates the suspicion that it is a focal demyelination. This indicates that the problem is to be referred to the nervous component rather than to the muscular one, therefore, our attention should focus on the type of focal demyelination, extent of damage and presumably localization of the damage. The differential diagnosis at this point focuses on the type and area of the demyelinating damage, for example, if it is a damage exclusively referred to the masseterine motor nerve or the motor nerve of the temporal muscle is also involved, important for treatment with botulinum endotoxin. To resolve this doubt it is necessary to evoke a heteronymous response from recording on the temporal muscle.
H-wave
The arrangement is similar to that previously described with regard to the with the variant that the temporal muscle is recorded simultaneously with the stimulation of the masseterine nerve in the intratemporal fossa by a bipolar needle electrode. The stimulation must be gradually adapted in order to evoke both a from the masseter that a heteronymous from the temporal muscle.
In our patient Mary Poppins, unfortunately, the neuromotor situation is quite complex and serious because to the infratemporal stimulation of the masseteral nerve we have a direct evoked response on the muscle ipsilateral to the stimulation (figure 10; ) and at the same time not a heteronymous response (figure 10; ) on the temporal muscle but rather a tonic asynchronous activity (Figure )
This neurophysiopathological phenomenon is called 'Ephaptic transmission' and allows us to confirm the presence of demyelinating lesions also of the motor nerve of the temporal muscle.
As previously mentioned and in order not to burden the topic, the detailed description of the 'Hephaptic' phenomenon will be treated in the chapter 'Encrypted code: Ephaptic transmission' in order to better understand the physiological responses of heteronymous by pathological ones.

Conclusions
Following this step by step path we have demonstrated a peripheral motor nerve injury as originally proposed by Kaufman.[5] Conduction studies have shown a slowing of conduction in the extracranial course of masticatory nerve fibers without a reduction in the amplitude of and obviously EMG signs of chronic denervation. The temporal muscle biopsy appeared histologically normal.
The absence of the jaw jerk on the diseased side indicates damage to the large diameter afferent fibers () from the neuromuscular spindles. A lesion of few afferents could easily abolish the jaw jerk.[6]
Muscle nerve damage would not be explained only because patients with Hemimasticatory Spasm (HMS) do not have sensory disturbances but also because they often only have spasms in one or two levator mandibular muscles. These observations argue against damage to the motor root or to the intracranial portion of the mandibular nerve where the motor bundles are closely grouped,[7] favoring damage to the individual muscle nerves that pass through the infratemporal fossa.
The mechanism of involvement of facial paroxysmal involuntary activity has been discussed by Kaufnan[5] and by Thompson and Carroll[8] who emphasized the close similarity between hemimasticatory and hemifacial spasm.
In EMG, these prolonged spasms fit perfectly into the description of cramps, that is, discharges of irregular motor units that progressively increase, leading to the recruitment of much of the muscle of synchronous discharges at speeds of 40 to 60 Hz.[9] Common to hemifacial spasm and cramps however, ectopic EMG activities can also be detected.
This could be responsible for the high frequency of EMG discharges at a frequency of 100-200 Hz and the synchronization of the entire muscle or multiple muscles, and post-activity. The synchronization could be explained by the lateral spread of discharges from adjacent nerve fibers,[10][11] generating a local re-excitation circuit. Posthumous EMG activity consists of paroxysmal discharges that may follow a voluntary orthodromic contraction or antidromic impulses,[12][13] and is attributed to self-excitation of the same axons after the passage of an impulse.
In our patient Mary Poppins we observed a synchronization of the whole or a large part of the muscle involved in the spasm (fig 10, EMG); the self-excitation is evidenced by the recording of the evoked discharges following the response of the stimulation of the chewing nerves (Fig. 10, E). These results support the hypothesis that spontaneous activity 'arises' in a demyelinated peripheral nerve, a phenomenon called hepaptic.[13]
In conclusion, the patient was affected by 'Hemimasticatory Spasm' mainly focused on the right masseter muscle but with indirect diffusion of the phenomenon to the right temporal muscle probably due to hepaptic activity due to the demyelination of the masticatory motor nerves in the infratemporal fossa. Botulinum endotoxin therapy was started immediately with total regression of the disease 10 years later.
(we will try to describe it in the chapter 'Crypted code: Ephaptic transmission' at the end of the section 'Hemasticatory spasm')
- ↑ Cruccu G, Truini A, Priori A, «Excitability of the human trigeminal motoneuronal pool and interactions with other brainstem reflex pathways», in J Physiol, The Physiological Society, 2001».
PMID:11230527 - PMCID:PMC2278464
DOI:10.1111/j.1469-7793.2001.0559i.x - ↑ 2.0 2.1 Frisardi G, «The use of transcranial stimulation in the fabrication of an occlusal splint», in J Prosthet Dent, Mosby, Inc - Elsevier, 1992».
PMID:1501190
DOI:10.1016/0022-3913(92)90345-b - ↑ Macaluso G, De Laat A. H-reflexes in masseter and temporalis muscle in man. Experimental Brain Research. 1995;107:315–320. [PubMed] [Google Scholar] [Ref list]
- ↑ G Frisardi, P Ravazzani, G Tognola, F Grandori. Electric versus magnetic transcranial stimulation of the trigeminal system in healthy subjects. Clinical applications in gnathology. J Oral Rehab.1997 Dec;24(12):920-8.doi: 10.1046/j.1365-2842.1997.00577.x.
- ↑ 5.0 5.1 Kaufman MD. Masticatory spasm in facial hemiatrophy. Ann Neurol 1980;7:585-7.
- ↑ Cruccu G, Inghilleri M, Fraioli B, Guidetti B, et al. Neurophysiologic assessment of trigeminal function after surgery for trigeminal neuralgia. Neurology 1987; 37:631-8.
- ↑ Pennisi E, Cruccu G, Manfredi M, Palladini G. Histometric study of myelinated fibers in the human trigeminal nerve. J Neurol Sci 1991;105:22-8.
- ↑ Thompson PD, Carroll WM. Hemimasticatory spasm: a peripheral paroxysmal cranial neuropathy? J Neurol NeurosurgPsychiatry 1983;46:274-6.
- ↑ Kimura J. Electrodiagnosis in diseases of nerve and muscle: principles and practice, 2nd edn. Philadelphia: FA Davis 1989.
- ↑ Nielsen VK. Pathophysiology of hemifacial spasm: II. Lateral spread of the supraorbital nerve reflex. Neurology 1984;34:427-31.
- ↑ Thompson PD. Stiff people. In Fahn S, Marsden CD, eds. Movement disorders 3. London: Butterworths, 1993: 367-99.
- ↑ Auger RG. Hemnifacial spasm: clinical and electrophysio- logic observations. Neurology 1979;29: 1261-72.
- ↑ 13.0 13.1 Nielsen VK. Pathophysiology of hemifacial spasm: I. Ephaptic transmission and ectopic excitation. Neurology 1984;34:418-26.
particularly focusing on the field of the neurophysiology of the masticatory system











![{\displaystyle \delta _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/cd35df3912a48e5b0b70d9cd5b2e1bee432c3272)
















![{\displaystyle \gamma _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/2f85d0ed73fa3e7903f0321e48668467c1277f4e)











![{\displaystyle \tau =[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/fbdc534cec0dcf1f070a551e40611eb83e8aca25)