Difference between revisions of "1° Clinical case: Hemimasticatory spasm"
m (Gianni moved page 1° Clinical case: Hemimasticatory spasm - en to 1° Clinical case: Hemimasticatory spasm) |
|
(No difference)
| |
Revision as of 10:55, 13 April 2023
| Other languages: |
In the previous chapters we have considered the diagnostic complexity in medicine taking into account especially some parameters such as the hidden variables that only the evolution of basic knowledge over time will allow us to identify and the difficulties in decoding the encrypted signal that the Central Nervous System sends to the external in the form of verbal language.
Last but not least, the limitations imposed by a deterministic mindset that reduces knowledge in specialist contexts by limiting its diagnostic capacity. An alternative mindset to deterministics that primarily considers a logic of fuzzy language and the important contribution of quantum probability would allow us to expand the scientific-clinical horizons and delve into a mesoscopic reality.
In this chapter, therefore, we will deal with the diagnosis of our Mary Poppins following the scientific-clinical process, evaluating the difficulties of implementation and the added value of the encrypted code identified in the hepaptic transmission.
Introduction
From what has been exposed in the previous chapters from the 'Introduction' to the 'Logic of medic language' chapters, beyond the complexity of the arguments and the vagueness of the verbal language, we found ourselves faced with a dilemma that of the context in which the patient is referred and in these cases for our poor Mary Poppins it seems to dominate the dental context, given the positive assertions reported by the clinical and laboratory tests performed on the patient.
(it would seem apparently but ......)
The clinical case of our poor Mary Poppins shows all the physiopathological and clinical complexity but above all a phenomenon of overlapping of propositions, statements and logical phrases in the dental and neurological context in which, one context obtains compatibility and coherence while the other incoherence.
Basically, given the compatibility and consistency of sentence (dental context) with the assertions derived from the clinical test reporting , consistently say that Orofacial Pain is caused by a Temporomandibular Disorder could become incompatible if another set of clinical statements were consistent with sentence (neurological context) and contextually opposite, from a diagnostic point of view, to
Therefore, there would be a source of logistical conflict between the two specialist contexts with inevitable diagnostic delay, also polluting the decryption process of the signal in the machine language of the Central Nervous System (CNS).
What will determine the access key for decoding the encrypted code in machine language (SNC) and will allow us to intercept a demarcation line will be an irrefutable clinical and / or laboratory data called , which will confirm or exclude the consistency of an assertion than the other. It is essential, at this point, a sentence (demarcation sentence) of the type will be:
Does Mary Poppins have a neuromotor disorder or a Temporomandibular Disorder?
We explain this step in detail:
Remember that da 'The logic of classical language' this shows :
- A set of sentences, and a number of other statements they are logically compatible if, and only if, the union between them it is consistent
- A set of sentences, and a number of other statements they are logically incompatible if, and only if, the union between them it is inconsistent
Significance of contexts
Now, for the dental context we will have the following sentences and assertions to which we give a numerical value to facilitate the treatment and that is where indicates' normality' and 'abnormality' and therefore positivity of the report:
Positive radiological report of the TMJ in Figure 2, Abnormality, positivity of the report
Positive CT report of the TMJ in Figure 3, Abnormality, positivity of the report
Positive axiographic report of the condylar traces in Figure 4, Abnormality, positivity of the report
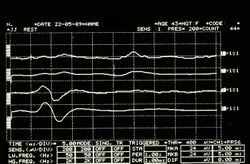
Asymmetric EMG interference pattern in Figure 5, Abnormality, positivity of the report
The sentence (dental context) with a number of other logically compatible assertions determine the union and coherence between them and are represented with a mathematical formalism to facilitate the diagnostic dialectic in the following way:
which represents the average of the individual statements reported. The average was designed because it can often happen that some tests give negative answers to which to give the value
The result in this case is and at the same time it derives the coherent statement of the sentence in which it is argued that the symptomatology of the patient Mary Poppins is determined by the presence of a DTMs.
(and it is precisely here that the contexts conflict)
In the neurological context, therefore, we will have the following sentences and assertions to which we give a numerical value to facilitate the treatment and that is where indicates 'normality' and 'abnormality' and therefore positivity of the report:
Absence of jaw jerk in Figures 6, Abnormality, positivity of the report
Absence of the silent masseterine period in Figures 7, Abnormality, positivity of the report
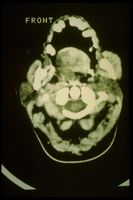
Hypertrophy of the right masseter on CT in Figures 8, Abnormality, positivity of the report
Now consequently also sentence with a number of other logically compatible statements determine the union and coherence between them and the formal representation will be similar to that of the dental context:
with contextual coherent affirmation of sentence in which it is argued that the symptomatology of the patient Mary Poppins has a neuromotor cause and the clinical consequences of a masticatory occlusal type are nothing other than a consequence of the neuropathic damage.
Demarcator of coherence
The is a representative clinical specific weight, complex to research and fine-tune because it varies from discipline to discipline and for pathologies, essential in order not to make logical assertions collide and in the diagnostic procedures and essential to initialize the decryption of the logic communication code. Basically it allows you to confirm the consistency of a union with respect to another and vice versa, giving greater weight to the severity of the statements and the report in the appropriate context.
Sometimes the physician is faced with a series of positive reports to which to give due weight, he must consider the positivity of a report that highlights, for example, an osteoarticular remodeling of the TMJ cannot have the same weight as a positivity of a report confirming a latency delay of a trigeminal reflex.
The weight of demarcation , therefore, gives more significance to the most serious assertions in the clinical context from which they derive and therefore beyond the positivity of the or assertions which in any case are always verified and respected, these must be multiplied by a where indicates 'Low severity' while 'High severity'.
In the neurological context, concerns the presence of delays and/or latency absence of the jaw jerk, duration and/or absence of the masseterine silent period as well as other parameters that for the moment it is not necessary to describe. A delay greater than the normative value or an absence of the aforementioned tests is considered as a serious and absolute specific weight corresponding to a dominant valence with respect to the other clinical context.
To recap we therefore have:
where
average of the value of clinical statements in the dental context and therefore
average of the value of clinical statements in the neurological context and therefore
low severity performance of the dental contextreporting of high severity of the neurological context
where the 'coherence marker '' will define the diagnostic path as follows
Once we have washed away the myriad of positively reported normative data, which generate conflicts between contexts, thanks to the coherence marker we have a much clearer and more linear picture on which to deepen the analysis of the functionality of the Central Nervous System. Consequently we can concentrate on intercepting the tests necessary to decrypt the machine language code that the SNC sends out converted into verbal language.
Ephaptic transmission
With a little effort and patience on the part of passionate readers who have followed the entire logical path, sometimes apparently off topic, we have reached a clinical picture in which the code to be decrypted is inherent in neuromotor damage. Consequently, the access keys to the code, the one that figuratively corresponds to the exact decryption algorithm, would correspond to the right choice of the neuromotor damage detector test.
This is a point where it is essential to infer the clinician's intuition because finding the right algorithm to decrypt the code, after the aforementioned filter steps that have been described to wash away the interference of assertions, means at least choosing the right dictionary, for example, that of the image (MR of the brain rather than the neck); acoustic and vestibular evoked potentials (if a vestibular scwannoma is suspected) or trigeminal electrophysiological study (if more than one trigeminal involvement is suspected).
In this clinical iter that we have presented, the choice of the clinician to follow the electrophysiological trigeminal roadmap from which the positivity of the assertions have already been derived, therefore, having already defined a picture of serious anomaly of absence of the jaw jerk and of the silent period masseterino on the right side of the patient will have to understand if the damage is intracranial or extracranial.
To do this, the clinician uses an electrical stimulation test of the masseter nerve in infratemporal fossa called on the masseter muscle with simultaneous recording of the heteronymous on the temporal muscle[1] and a bilateral transcranial electrical stimulation of the trigeminal motor roots called, precisely, [2]
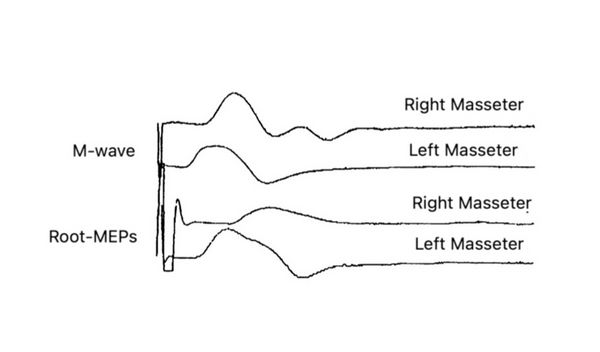
M-wave
The right masseter nerve was electrically stimulated in the infratemporal fossa (see clinical procedure chapter: Encrypted code: Ephaptic transmission) with a technique similar to that described by Macaluso & De Laat (1995).[3] Square cathode pulses (0.1 ms) generated by an electrical stimulator (Neuropack X1, Nihon Kohden Corporation, Tokyo, Japan) were delivered through a Teflon-coated monopolar needle electrode (TECA 902-DMG25, 53534) with a tip non-isolated (diameter 0.36 mm; area 0.28 mm2) inserted 1.5 cm through the skin below the zygomatic arch and anterior to the temporomandibular joint in the infratemporal fossa with electrical shocks of 0.5 - 5 mA, and 0.1 ms. The anode was a surface non-polarizable Ag-AgCl disc electrode (OD 9.0 mm) positioned over the ipsilateral ear lobe. Electrical stimulation of the masseter nerve never produced pain, and the subjects only perceived muscle contraction. The correct position of the stimulation electrodes was monitored throughout the experimental session by checking online the size of the M wave in the masseter muscle. The signals were recorded by placing surface electrodes on the masseter and temporal muscles and filtered at 10-2000Hz and by concentric needle electrodes inserted into the anterior temporal muscle.
bRoot-MEPs
The trigeminal root was stimulated transcrally through high voltage, low impedance through an electrical stimulator (Neuropack X1, Nihon Kohden Corporation, Tokyo, Japan)) with the anode electrode positioned at the apex and the cathode approximately 10 cm laterally from the apex along a line vertex acoustic meatus. The electric field is believed to excite the trigeminal motor nerve fibers via the trancranial route, near their exit from the skull.[2][4] Also in this case, the response in the right masseter was markedly delayed (3.5 ms on the right side 2 ms on the left and dispersed. amplitude of the M-wave.
Having highlighted, through the execution of the and test, a delay in the conduction speed of the trigeminal nerve fibers generates the suspicion that it is a focal demyelination. This indicates that the problem is to be referred to the nervous component rather than to the muscular one, therefore, our attention should focus on the type of focal demyelination, extent of damage and presumably localization of the damage. The differential diagnosis at this point focuses on the type and area of the demyelinating damage, for example, if it is a damage exclusively referred to the masseterine motor nerve or the motor nerve of the temporal muscle is also involved, important for treatment with botulinum endotoxin. To resolve this doubt it is necessary to evoke a heteronymous response from recording on the temporal muscle.
H-wave
The arrangement is similar to that previously described with regard to the with the variant that the temporal muscle is recorded simultaneously with the stimulation of the masseterine nerve in the intratemporal fossa by a bipolar needle electrode. The stimulation must be gradually adapted in order to evoke both a from the masseter that a heteronymous from the temporal muscle.
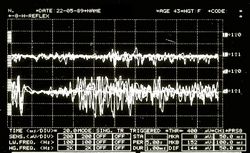
In our patient Mary Poppins, unfortunately, the neuromotor situation is quite complex and serious because to the infratemporal stimulation of the masseteral nerve we have a direct evoked response on the muscle ipsilateral to the stimulation (figure 10; ) and at the same time not a heteronymous response (figure 10; ) on the temporal muscle but rather a tonic asynchronous activity (Figure )
This neurophysiopathological phenomenon is called 'Ephaptic transmission' and allows us to confirm the presence of demyelinating lesions also of the motor nerve of the temporal muscle.
As previously mentioned and in order not to burden the topic, the detailed description of the 'Hephaptic' phenomenon will be treated in the chapter 'Encrypted code: Ephaptic transmission' in order to better understand the physiological responses of heteronymous by pathological ones.

Conclusions
Following this step by step path we have demonstrated a peripheral motor nerve injury as originally proposed by Kaufman.[5] Conduction studies have shown a slowing of conduction in the extracranial course of masticatory nerve fibers without a reduction in the amplitude of and obviously EMG signs of chronic denervation. The temporal muscle biopsy appeared histologically normal.
The absence of the jaw jerk on the diseased side indicates damage to the large diameter afferent fibers () from the neuromuscular spindles. A lesion of few afferents could easily abolish the jaw jerk.[6]
Muscle nerve damage would not be explained only because patients with Hemimasticatory Spasm (HMS) do not have sensory disturbances but also because they often only have spasms in one or two levator mandibular muscles. These observations argue against damage to the motor root or to the intracranial portion of the mandibular nerve where the motor bundles are closely grouped,[7] favoring damage to the individual muscle nerves that pass through the infratemporal fossa.
The mechanism of involvement of facial paroxysmal involuntary activity has been discussed by Kaufnan[5] and by Thompson and Carroll[8] who emphasized the close similarity between hemimasticatory and hemifacial spasm.
In EMG, these prolonged spasms fit perfectly into the description of cramps, that is, discharges of irregular motor units that progressively increase, leading to the recruitment of much of the muscle of synchronous discharges at speeds of 40 to 60 Hz.[9] Common to hemifacial spasm and cramps however, ectopic EMG activities can also be detected.
This could be responsible for the high frequency of EMG discharges at a frequency of 100-200 Hz and the synchronization of the entire muscle or multiple muscles, and post-activity. The synchronization could be explained by the lateral spread of discharges from adjacent nerve fibers,[10][11] generating a local re-excitation circuit. Posthumous EMG activity consists of paroxysmal discharges that may follow a voluntary orthodromic contraction or antidromic impulses,[12][13] and is attributed to self-excitation of the same axons after the passage of an impulse.
In our patient Mary Poppins we observed a synchronization of the whole or a large part of the muscle involved in the spasm (fig 10, EMG); the self-excitation is evidenced by the recording of the evoked discharges following the response of the stimulation of the chewing nerves (Fig. 10, E). These results support the hypothesis that spontaneous activity 'arises' in a demyelinated peripheral nerve, a phenomenon called hepaptic.[13]
In conclusion, the patient was affected by 'Hemimasticatory Spasm' mainly focused on the right masseter muscle but with indirect diffusion of the phenomenon to the right temporal muscle probably due to hepaptic activity due to the demyelination of the masticatory motor nerves in the infratemporal fossa. Botulinum endotoxin therapy was started immediately with total regression of the disease 10 years later.
(we will try to describe it in the chapter 'Crypted code: Ephaptic transmission' at the end of the section 'Hemasticatory spasm')
- ↑ Cruccu G, Truini A, Priori A, «Excitability of the human trigeminal motoneuronal pool and interactions with other brainstem reflex pathways», in J Physiol, The Physiological Society, 2001».
PMID:11230527 - PMCID:PMC2278464
DOI:10.1111/j.1469-7793.2001.0559i.x - ↑ 2.0 2.1 Frisardi G, «The use of transcranial stimulation in the fabrication of an occlusal splint», in J Prosthet Dent, Mosby, Inc - Elsevier, 1992».
PMID:1501190
DOI:10.1016/0022-3913(92)90345-b - ↑ Macaluso G, De Laat A. H-reflexes in masseter and temporalis muscle in man. Experimental Brain Research. 1995;107:315–320. [PubMed] [Google Scholar] [Ref list]
- ↑ G Frisardi, P Ravazzani, G Tognola, F Grandori. Electric versus magnetic transcranial stimulation of the trigeminal system in healthy subjects. Clinical applications in gnathology. J Oral Rehab.1997 Dec;24(12):920-8.doi: 10.1046/j.1365-2842.1997.00577.x.
- ↑ 5.0 5.1 Kaufman MD. Masticatory spasm in facial hemiatrophy. Ann Neurol 1980;7:585-7.
- ↑ Cruccu G, Inghilleri M, Fraioli B, Guidetti B, et al. Neurophysiologic assessment of trigeminal function after surgery for trigeminal neuralgia. Neurology 1987; 37:631-8.
- ↑ Pennisi E, Cruccu G, Manfredi M, Palladini G. Histometric study of myelinated fibers in the human trigeminal nerve. J Neurol Sci 1991;105:22-8.
- ↑ Thompson PD, Carroll WM. Hemimasticatory spasm: a peripheral paroxysmal cranial neuropathy? J Neurol NeurosurgPsychiatry 1983;46:274-6.
- ↑ Kimura J. Electrodiagnosis in diseases of nerve and muscle: principles and practice, 2nd edn. Philadelphia: FA Davis 1989.
- ↑ Nielsen VK. Pathophysiology of hemifacial spasm: II. Lateral spread of the supraorbital nerve reflex. Neurology 1984;34:427-31.
- ↑ Thompson PD. Stiff people. In Fahn S, Marsden CD, eds. Movement disorders 3. London: Butterworths, 1993: 367-99.
- ↑ Auger RG. Hemnifacial spasm: clinical and electrophysio- logic observations. Neurology 1979;29: 1261-72.
- ↑ 13.0 13.1 Nielsen VK. Pathophysiology of hemifacial spasm: I. Ephaptic transmission and ectopic excitation. Neurology 1984;34:418-26.
particularly focusing on the field of the neurophysiology of the masticatory system











![{\displaystyle \delta _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/cd35df3912a48e5b0b70d9cd5b2e1bee432c3272)
















![{\displaystyle \gamma _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/2f85d0ed73fa3e7903f0321e48668467c1277f4e)











![{\displaystyle \tau =[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/fbdc534cec0dcf1f070a551e40611eb83e8aca25)