Difference between revisions of "Store:EMen03"
Tags: Reverted Mobile web edit Mobile edit Visual edit |
Tags: Reverted Mobile web edit Mobile edit Visual edit |
||
| Line 1: | Line 1: | ||
=== | === Multiple sclerosis and trigeminal reflexes === | ||
We must make an additional premise about axonal demyelination in multiple sclerosis. From a study by Joanna Kamińska andt al.<ref>Joanna Kamińska, Olga M Koper, Kinga Piechal, Halina Kemona . [https://pubmed.ncbi.nlm.nih.gov/28665284/ Multiple sclerosis - etiology and diagnostic potential].Postepy Hig Med Dosw. 2017 Jun 30;71(0):551-563.doi: 10.5604/01.3001.0010.3836. | |||
</ref> | </ref> It appears that multiple sclerosis (MS) is a chronic inflammatory and demyelinating disease of autoimmune origin. The main agents responsible for the development of MS include exogenous, environmental and genetic factors. MS is characterized by multifocal and temporally dispersed damage to the central nervous system (CNS) leading to axonal damage. Among the clinical courses of MS we can distinguish relapsing-remitting multiple sclerosis (RRMS), secondary progressive multiple sclerosis (MSPS), primary progressive multiple sclerosis (PPMS) and relapsing progressive multiple sclerosis (PRMS). Depending on the severity of the signs and symptoms, MS can be described as either benign MS or malignant MS. The diagnosis of MS is based on the McDonald's diagnostic criteria, which link the clinical manifestation with the characteristic lesions demonstrated by magnetic resonance imaging (MRI), cerebrospinal fluid (CSF) analysis, and visual evoked potentials. | ||
It should be noted that despite the enormous progress in MS and the availability of different diagnostic methods, this disease still represents a diagnostic challenge. It may be due to the fact that MS has a different clinical course and a single test is missing, which would have the appropriate diagnostic sensitivity and specificity for rapid and accurate diagnosis. | |||
<blockquote> | <blockquote>Precisely in reference to this last observation we must point out another significant piece of information arising from a study by S K Yates and W F Brown<ref>S K Yates, W F Brown. The human jaw jerk: electrophysiologic methods to measure the latency, normal values, and changes in multiple sclerosis.Neurology. 1981 May;31(5):632-4.doi: 10.1212/wnl.31.5.632. | ||
</ref> | </ref> in which we read that the jaw masseter reflex is present in all control subjects, but is generally absent in sclerosis patients. defined multiple (SM). In some MS patients, latency was prolonged. However, abnormalities in the jaw reflex are less common than blink reflex responses to supraorbital nerve stimulation. However, there have been patients in whom the reflex blinks were normal but the jaw jerk responses were abnormal. The latter observation suggests that the jaw reflex may sometimes be useful in detecting brainstem lesions in MS.</blockquote>But at this point the doubt becomes true in the sense: what should we think of the anomalies of the trigeminal reflexes highlighted in our Mary Poppins? Could we be facing a form of 'Multiple Sclerosis'? How do we distinguish the location of any unwinding, Central or Peripheral in the trigeminal nervous system? | ||
<center> | <center> | ||
<gallery widths="350" heights="200" perrow="4" slideshow""=""> | <gallery widths="350" heights="200" perrow="4" slideshow""=""> | ||
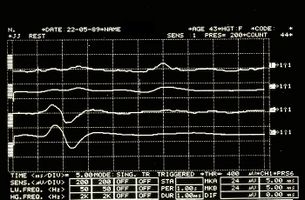
File:Spasmo emimasticatorio JJ.jpg| | File:Spasmo emimasticatorio JJ.jpg|Figure 6: Electrophysiologically detected jaw jerk in the right (upper traces) and left (lower traces) masseters | ||
File:Spasmo emimasticatorio SP.jpg| | File:Spasmo emimasticatorio SP.jpg|Figure 7: Electrophysiologically detected mechanical silent period in the right (upper overlapping traces) and left (lower overlapping traces) masseters | ||
</gallery> | </gallery> | ||
</center> | </center> | ||
Revision as of 10:10, 1 May 2023
Multiple sclerosis and trigeminal reflexes
We must make an additional premise about axonal demyelination in multiple sclerosis. From a study by Joanna Kamińska andt al.[1] It appears that multiple sclerosis (MS) is a chronic inflammatory and demyelinating disease of autoimmune origin. The main agents responsible for the development of MS include exogenous, environmental and genetic factors. MS is characterized by multifocal and temporally dispersed damage to the central nervous system (CNS) leading to axonal damage. Among the clinical courses of MS we can distinguish relapsing-remitting multiple sclerosis (RRMS), secondary progressive multiple sclerosis (MSPS), primary progressive multiple sclerosis (PPMS) and relapsing progressive multiple sclerosis (PRMS). Depending on the severity of the signs and symptoms, MS can be described as either benign MS or malignant MS. The diagnosis of MS is based on the McDonald's diagnostic criteria, which link the clinical manifestation with the characteristic lesions demonstrated by magnetic resonance imaging (MRI), cerebrospinal fluid (CSF) analysis, and visual evoked potentials.
It should be noted that despite the enormous progress in MS and the availability of different diagnostic methods, this disease still represents a diagnostic challenge. It may be due to the fact that MS has a different clinical course and a single test is missing, which would have the appropriate diagnostic sensitivity and specificity for rapid and accurate diagnosis.
Precisely in reference to this last observation we must point out another significant piece of information arising from a study by S K Yates and W F Brown[2] in which we read that the jaw masseter reflex is present in all control subjects, but is generally absent in sclerosis patients. defined multiple (SM). In some MS patients, latency was prolonged. However, abnormalities in the jaw reflex are less common than blink reflex responses to supraorbital nerve stimulation. However, there have been patients in whom the reflex blinks were normal but the jaw jerk responses were abnormal. The latter observation suggests that the jaw reflex may sometimes be useful in detecting brainstem lesions in MS.
But at this point the doubt becomes true in the sense: what should we think of the anomalies of the trigeminal reflexes highlighted in our Mary Poppins? Could we be facing a form of 'Multiple Sclerosis'? How do we distinguish the location of any unwinding, Central or Peripheral in the trigeminal nervous system?
- ↑ Joanna Kamińska, Olga M Koper, Kinga Piechal, Halina Kemona . Multiple sclerosis - etiology and diagnostic potential.Postepy Hig Med Dosw. 2017 Jun 30;71(0):551-563.doi: 10.5604/01.3001.0010.3836.
- ↑ S K Yates, W F Brown. The human jaw jerk: electrophysiologic methods to measure the latency, normal values, and changes in multiple sclerosis.Neurology. 1981 May;31(5):632-4.doi: 10.1212/wnl.31.5.632.