Difference between revisions of "Store:EMen03"
Tags: Reverted Mobile web edit Mobile edit Visual edit |
Tags: Manual revert Visual edit |
||
| (3 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
=== | === Multiple sclerosis and trigeminal reflexes === | ||
We must make a further premise concerning axonal demilienization in multiple sclerosis. From a study by Joanna Kamińska et al.<ref>Joanna Kamińska, Olga M Koper, Kinga Piechal, Halina Kemona . [https://pubmed.ncbi.nlm.nih.gov/28665284/ Multiple sclerosis - etiology and diagnostic potential].Postepy Hig Med Dosw. 2017 Jun 30;71(0):551-563.doi: 10.5604/01.3001.0010.3836. | |||
</ref> | </ref> it appears that multiple sclerosis (MS) is a chronic inflammatory and demyelinating disease of autoimmune origin. The main agents responsible for the development of MS include exogenous, environmental and genetic factors. MS is characterized by multifocal and temporally scattered damage of the central nervous system (CNS) leading to axonal damage. Among the clinical courses of MS we can distinguish relapsing-remitting multiple sclerosis (RRMS), secondary progressive multiple sclerosis (SPSM), primary progressive multiple sclerosis (PPMS) and relapsing progressive multiple sclerosis (RPMS). Depending on the severity of the signs and symptoms, MS can be described as benign MS or malignant MS. Diagnosis of MS is based on McDonald's diagnostic criteria, which link clinical manifestation with characteristic lesions demonstrated by magnetic resonance imaging (MRI), cerebrospinal fluid (CSF) analysis, and visual evoked potentials. | ||
It should be emphasized that despite the enormous progress in MS and the availability of different diagnostic methods, this disease still represents a diagnostic challenge. It may result from the fact that MS has a different clinical course and a single test is missing, which would be of appropriate diagnostic sensitivity and specificity for rapid and accurate diagnosis. | |||
<blockquote> | <blockquote>Precisely in reference to this last observation we must point out another significant data that emerged from a study by S K Yates and W F Brown<ref>S K Yates, W F Brown. The human jaw jerk: electrophysiologic methods to measure the latency, normal values, and changes in multiple sclerosis.Neurology. 1981 May;31(5):632-4.doi: 10.1212/wnl.31.5.632. | ||
</ref> | </ref> in which we read that the jaw jerk of the masseter is present in all control subjects but commonly absent in patients with sclerosis. multiple defined (SM). In some MS patients, the latency was prolonged. Abnormalities in jaw jerk, however, are less common than blink reflex responses to supraorbital nerve stimulation. However, there have been patients in whom the reflex blinks were normal but the jaw jerk responses were abnormal. The latest observation suggests that jaw jerk may occasionally be useful in detecting brain stem injury in MS.</blockquote>But at this point the doubt becomes reality in the sense: what should we think of the anomalies of the trigeminal reflexes highlighted in our Mary Poppins? Could we be facing a form of 'Multiple Sclerosis? How do we distinguish the location of any demienization, Central or Peripheral in the trigeminal nervous system? | ||
<center> | <center> | ||
<gallery widths="350" heights="200" perrow="4" slideshow""=""> | <gallery widths="350" heights="200" perrow="4" slideshow""=""> | ||
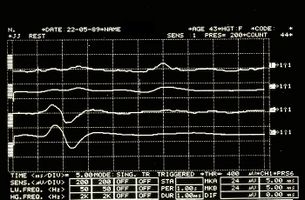
File:Spasmo emimasticatorio JJ.jpg| | File:Spasmo emimasticatorio JJ.jpg|'''Figure 6:''' Jaw jerk detected electrophysiologically on the right (upper traces) and left (lower traces) masseters | ||
File:Spasmo emimasticatorio SP.jpg| | File:Spasmo emimasticatorio SP.jpg|'''Figure 7:''' Period of mechanical silence detected electrophysiologically on the right (upper overlapping traces) and left (lower overlapping traces) masseters | ||
</gallery> | </gallery> | ||
</center> | </center> | ||
Latest revision as of 11:44, 1 May 2023
Multiple sclerosis and trigeminal reflexes
We must make a further premise concerning axonal demilienization in multiple sclerosis. From a study by Joanna Kamińska et al.[1] it appears that multiple sclerosis (MS) is a chronic inflammatory and demyelinating disease of autoimmune origin. The main agents responsible for the development of MS include exogenous, environmental and genetic factors. MS is characterized by multifocal and temporally scattered damage of the central nervous system (CNS) leading to axonal damage. Among the clinical courses of MS we can distinguish relapsing-remitting multiple sclerosis (RRMS), secondary progressive multiple sclerosis (SPSM), primary progressive multiple sclerosis (PPMS) and relapsing progressive multiple sclerosis (RPMS). Depending on the severity of the signs and symptoms, MS can be described as benign MS or malignant MS. Diagnosis of MS is based on McDonald's diagnostic criteria, which link clinical manifestation with characteristic lesions demonstrated by magnetic resonance imaging (MRI), cerebrospinal fluid (CSF) analysis, and visual evoked potentials.
It should be emphasized that despite the enormous progress in MS and the availability of different diagnostic methods, this disease still represents a diagnostic challenge. It may result from the fact that MS has a different clinical course and a single test is missing, which would be of appropriate diagnostic sensitivity and specificity for rapid and accurate diagnosis.
Precisely in reference to this last observation we must point out another significant data that emerged from a study by S K Yates and W F Brown[2] in which we read that the jaw jerk of the masseter is present in all control subjects but commonly absent in patients with sclerosis. multiple defined (SM). In some MS patients, the latency was prolonged. Abnormalities in jaw jerk, however, are less common than blink reflex responses to supraorbital nerve stimulation. However, there have been patients in whom the reflex blinks were normal but the jaw jerk responses were abnormal. The latest observation suggests that jaw jerk may occasionally be useful in detecting brain stem injury in MS.
But at this point the doubt becomes reality in the sense: what should we think of the anomalies of the trigeminal reflexes highlighted in our Mary Poppins? Could we be facing a form of 'Multiple Sclerosis? How do we distinguish the location of any demienization, Central or Peripheral in the trigeminal nervous system?
- ↑ Joanna Kamińska, Olga M Koper, Kinga Piechal, Halina Kemona . Multiple sclerosis - etiology and diagnostic potential.Postepy Hig Med Dosw. 2017 Jun 30;71(0):551-563.doi: 10.5604/01.3001.0010.3836.
- ↑ S K Yates, W F Brown. The human jaw jerk: electrophysiologic methods to measure the latency, normal values, and changes in multiple sclerosis.Neurology. 1981 May;31(5):632-4.doi: 10.1212/wnl.31.5.632.